
When a person mixes heroin with cocaine, they may seem anxious, uncoordinated, stupored, and drowsy. This mixture of depressant and stimulant is referred to as a speedball. A lot of people concurrently use heroin and cocaine to counter any side-effects from either drug, but it can also result in consequences such as respiratory failure, overdose, and coma.
What Is A Speedball And Why Is It Dangerous?
 A speedball refers to a mixture of depressants and stimulants; it’s a form of polysubstance abuse. A few examples of a speedballing are alprazolam with methamphetamine, alcohol with amphetamines, or the most common speedball, heroin with cocaine.
A speedball refers to a mixture of depressants and stimulants; it’s a form of polysubstance abuse. A few examples of a speedballing are alprazolam with methamphetamine, alcohol with amphetamines, or the most common speedball, heroin with cocaine.
People may use heroin with cocaine for the intense rush, or to minimize the negative side-effects or “come-down.” But the reality is the effect that mixing heroin with cocaine has on the body is unpredictable, and can be fatal.
How Cocaine Works
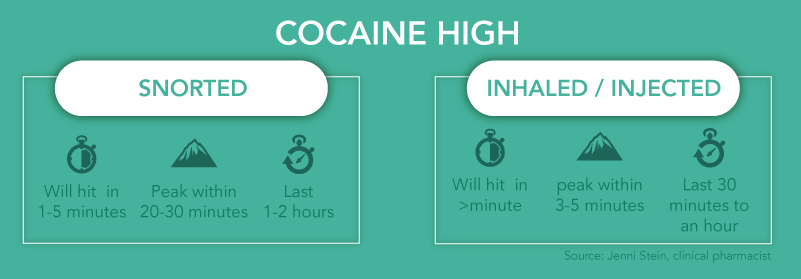
Cocaine works by stimulating a person’s central nervous system. It causes a flush of dopamine in a their brain, and increases their heart rate. The euphoric effect makes the user feel energetic, extremely happy, and often sleepless. Cocaine also acts on the parasympathetic nervous system which is responsible for regulating a person’s fight or flight response.
How Heroin Works
Heroin, on the other hand, works by depressing the central nervous system. Once it’s in the blood stream, heroin rushes to the brain and binds to opioid receptors—these are responsible for feelings of pain and pleasure, but also affect breathing, sleeping, and heart rate. Unlike cocaine, heroin affects the sympathetic nervous system, which is responsible for the body’s rest and digestion.
Mixing Heroin With Cocaine
When cocaine and heroin are mixed, their opposite effects can create a system debacle. This is because when both the sympathetic and parasympathetic systems mentioned above, are attacked, the brain responds by sending a mixed signal of what to do. Another, perhaps more practical danger is that the effects of cocaine wear off much faster than heroin, which can easily result in respiratory failure.
 Most of the time heroin and cocaine are diluted with non mood altering substances such as starch, sugar, flour, powdered milk, talcum powder, or even rat poisoning. So there isn’t always a way to tell what either drug has been cut with, thus the purity of each drug isn’t always clear. An amount that proved to be “safe” last time someone mixed heroin and cocaine, could be a fatal dose this time.
Most of the time heroin and cocaine are diluted with non mood altering substances such as starch, sugar, flour, powdered milk, talcum powder, or even rat poisoning. So there isn’t always a way to tell what either drug has been cut with, thus the purity of each drug isn’t always clear. An amount that proved to be “safe” last time someone mixed heroin and cocaine, could be a fatal dose this time.
In 2015, heroin alone killed 12,989 people. That same year, cocaine killed 6,784 people. From 2010-2015, heroin and cocaine related deaths more than doubled with a combined total that escalated from 8,408 deaths in 2010 up to 21,823 deaths in 2015.
Mixing cocaine and heroin isn’t only dangerous, it’s part of a growing epidemic in the United States. Without a serious change, and the right help, a lot more lives may be lost to addiction.
Signs Of Speedball Use
Some of the signs of speedballing will be harder to point out than others, but it may help to be able to recognize the signs of heroin and cocaine abuse.
That’s because many of the side-effects of heroin and cocaine are, “associated with the abuse of either one individually,” (NIDA for Teens).
The side-effects of speedballing heroin and cocaine may include:
- anxiety
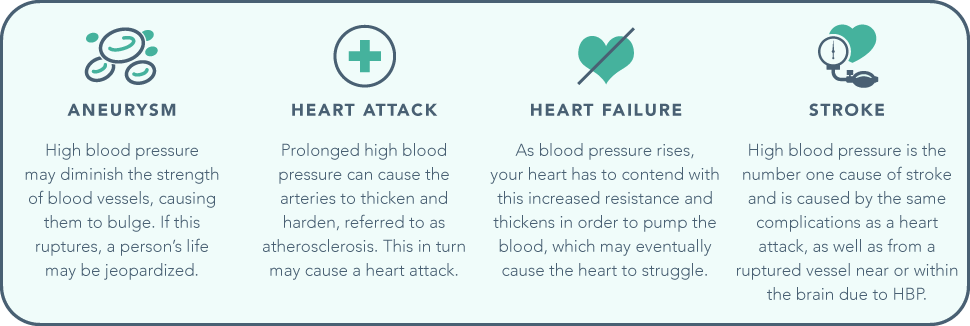
- high blood pressure
- strong or irregular heartbeat
- drowsiness
- suppression of breathing
- general confusion
- incoherence
- blurred vision
- stupor
- drowsiness
- paranoia
- mental impairment
- uncontrolled and uncoordinated motor skills
- risk of death from:
- stroke
- heart attack
- aneurysm
- respiratory failure
Why Mix Heroin With Cocaine?
The reasons that someone mixes heroin with cocaine can vary, but there are a lot of people who inject a mixture of the two to chase the perfect euphoria. Others may combine the heroin with cocaine to counter the drug side-effects like anxiety, depression, or even a crash.
Heroin is a mentally and physically addictive drug that can be extremely difficult to quit cold turkey. A lot of people are met with the challenge of intense mental and physical withdrawals when they finally do stop using heroin.

Everybody’s different, and there so there’s no clear-cut reason that people will mix depressants and stimulants. There are also people who use cocaine as a sort self-medication for heroin withdrawal.
Heroin withdrawal can include the following symptoms:
- restlessness
- severe muscle and bone pain
- sleep problems
- diarrhea and vomiting
- cold flashes with goose bumps
- uncontrollable leg movements
- severe heroin cravings
(NIDA)
Treatment For Addiction To Heroin And Cocaine
Finding an evidence-based inpatient rehab center is the usually the best first step to get help for someone struggling with an addiction to heroin and/or cocaine.
Some of the unique treatment programs offered at rehab centers include:
- Evalulation
- Detoxification
- Medication-Assisted Therapy
- Cognitive Behavioral Therapy
- Dialectical Behavior Therapy
- Contingency Management
- Individual and Group Therapy
Find An Addiction Treatment Program That Works
If you or someone you love is struggling with an addiction to cocaine and heroin, contact DrugRehab.org to speak to an addiction treatment specialist about how to get help. Your recovery is important to us, and your call will be completely confidential.
For More Information Related to “Signs of Speedball (Heroin with Cocaine) Use” Be Sure To Check Out These Additional Resources From DrugRehab.org:
- Gray Death Heroin Abuse In The United States
- What Are The Most Potent Opioids In The United States?
- What is the Difference Between Cocaine and Crack?
- Heroin and Alcohol: A Deadly Combination
- Risks Associated with Snorting Heroin (Insufflation)
Sources
National Institute on Drug Abuse: National Center for Health Statistics – Overdose Death Rates
National Institute on Drug Abuse – Cocaine
National Institute on Drug Abuse – Heroin
National Institute on Drug Abuse – How Effective is Drug Addiction Treatment?
NIDA for Teens – Real Teens Ask About Speedballs













 Overall, benzodiazepine use was almost twice as prevalent in women as it was in men. This could be due to a wider social acceptance of women speaking with a psychiatrist about emotional issues than men, however it could also be linked to other environmental factors.
Overall, benzodiazepine use was almost twice as prevalent in women as it was in men. This could be due to a wider social acceptance of women speaking with a psychiatrist about emotional issues than men, however it could also be linked to other environmental factors.

 Since then the coca plant has grown in popularity among the rest of the world, especially since
Since then the coca plant has grown in popularity among the rest of the world, especially since 
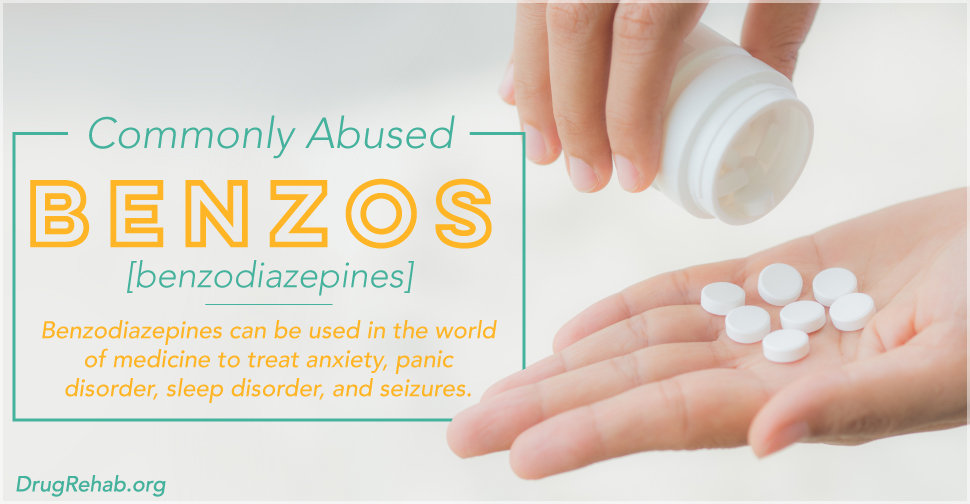
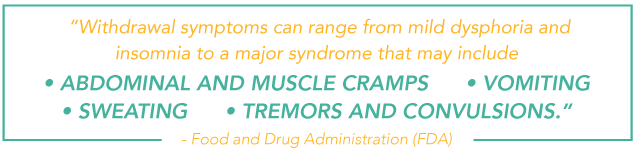
 The FDA sums it up perfectly, “abuse is characterized by misuse of the drug for nonmedical purposes, often in combination with other psychoactive substances. Physical dependence is a state of adaptation that is manifested by a specific withdrawal syndrome that can be produced by abrupt cessation, rapid dose reduction, decreasing blood level of the drug and/or administration of an antagonist…Tolerance is a state of adaptation in which exposure to a drug induces changes that result in a diminution of one or more of the drug’s effects over time.”
The FDA sums it up perfectly, “abuse is characterized by misuse of the drug for nonmedical purposes, often in combination with other psychoactive substances. Physical dependence is a state of adaptation that is manifested by a specific withdrawal syndrome that can be produced by abrupt cessation, rapid dose reduction, decreasing blood level of the drug and/or administration of an antagonist…Tolerance is a state of adaptation in which exposure to a drug induces changes that result in a diminution of one or more of the drug’s effects over time.”

 Mayo cites various risk factors that may put an individual at a heightened risk for HBP, including: age, family history, weight gain (becoming overweight or obese), physical inactivity, potassium or vitamin d intake is too low, sodium intake is too high, race, stress, and various other chronic health conditions. Additionally, those who use tobacco or consume an excess of alcohol face increased risks. For individuals experiencing these factors, the necessity in gaining control over their drug abuse is even more pressing. If a person already has a preexisting hypertension, the risk is compounded, and made more dangerous, by the drug abuse.
Mayo cites various risk factors that may put an individual at a heightened risk for HBP, including: age, family history, weight gain (becoming overweight or obese), physical inactivity, potassium or vitamin d intake is too low, sodium intake is too high, race, stress, and various other chronic health conditions. Additionally, those who use tobacco or consume an excess of alcohol face increased risks. For individuals experiencing these factors, the necessity in gaining control over their drug abuse is even more pressing. If a person already has a preexisting hypertension, the risk is compounded, and made more dangerous, by the drug abuse.
 Autism is much more common today than it was in past decades. The current number of children affected by autism is a ten-fold increase from forty years ago, according to Psychology Today. Research suggests autism gets its start in early brain development; one of the suggested ways to prevent autism for pregnant mothers is a diet high in folic acid. However, autism may be diagnosed in children two to three years of age—when symptoms tend to become obvious. Autism is also more common in boys than in girls.
Autism is much more common today than it was in past decades. The current number of children affected by autism is a ten-fold increase from forty years ago, according to Psychology Today. Research suggests autism gets its start in early brain development; one of the suggested ways to prevent autism for pregnant mothers is a diet high in folic acid. However, autism may be diagnosed in children two to three years of age—when symptoms tend to become obvious. Autism is also more common in boys than in girls. Autism is not typically associated with alcohol or drug abuse. Psychology Today explains that people with autism are traditionally not drawn to alcohol abuse because they tend to have a “preference for low risk and avoidance of social situations.” But the newest findings point to a heightened risk of addiction for those with autism. When two disorders occur together, they are called
Autism is not typically associated with alcohol or drug abuse. Psychology Today explains that people with autism are traditionally not drawn to alcohol abuse because they tend to have a “preference for low risk and avoidance of social situations.” But the newest findings point to a heightened risk of addiction for those with autism. When two disorders occur together, they are called  The goal for those with autism is often to move them into a manageable state of the disorder, and some reach this level. For those who don’t, and who develop addiction to drugs or alcohol, treatment is the best help available.
The goal for those with autism is often to move them into a manageable state of the disorder, and some reach this level. For those who don’t, and who develop addiction to drugs or alcohol, treatment is the best help available.