Along with intravenous injection, drugs like cocaine, steroids and heroin can be intradermally, subcutaneously and intramuscularly injected—also known as “skin-popping.” These types of drug injections can lead to health problems, euphoria, overdose, and amputations. Drug rehab centers can help a person safely begin recovery and stop abusing drugs.
Skin-popping is a method used to inject illicit substances like heroin and other opiates, cocaine, anabolic steroids, barbiturates, and some medications. Over the years, methods for using drugs have become more effective and easier. Skin-popping may be an easy method, but is just as dangerous as any other method and has potential to lead to serious skin conditions and other health complications.
What Is Skin-Popping?
Skin-popping is also known as subcutaneous or intradermal injection. It’s a preferred method of using black tar heroin, cocaine, and anabolic steroids. Intradermal injection is the introduction of a drug between the skin and fat just below the surface, and subcutaneous is injection of a drug into the tissue layers just beneath the layers of skin. A drug doesn’t work as quickly through intradermal or subcutaneous injection as it does from injecting it into the veins, directly into the bloodstream.
Why Skin-Popping?
There are a lot of reasons that people prefer not to inject chemicals directly into their veins. “For some, trying to hit a vein gets so frustrating that they just give up and shoot anywhere they can. Some do it because drugs absorb more slowly this way. Muscling and skin-popping give you less of a ‘rush,’ but the effects of the drug may last longer” (Public Health Seattle and King County).

People will also switch to skin-popping if frequent intravenous injections have led to hardened or scarred skin and the veins are no longer easily accessible. According to the U.S. National Library of Medicine (NLM), the most frequently used sites for injection are “the neck, supraclavicular region and the thorax.”
Some addicted individuals may be at the point that they aren’t so concerned about the rush, but more about the withdrawal that comes when they stop using the drugs.
Most Frequently Injected Drugs
The substances most commonly used for intradermal and subcutaneous injection are heroin and other opiates, cocaine, anabolic steroids, and sometimes barbiturates. Some of these substances are more dangerous and more addictive than others, but neither intravenous, nor intradermal, nor intramuscular injection is considered a safe alternative to use them.
“All three have serious risks. All three put you at great risk for blood-borne infections like HIV and Hepatitis B and C. Although muscling and skin-popping may cause more abscesses and skin infections, shooting into a vein may be more likely to cause serious long-term illnesses like endocarditis (heart valve infection)” (Public Health Seattle and King County).
Intradermal And Subcutaneous Substance Abuse
Intradermal means “within the skin” and subcutaneous means “under the skin.” In either case, they’re types of skin-popping, and can lead to different health problems and skin conditions. Subcutaneous injection goes deeper than intradermal but not as deep as intramuscular. More specifically, subcutaneous injections are inserted into a layer of skin just before the muscle.
Intradermally Injecting Cocaine
Cocaine is a stimulant that has a serious impact on a person’s nervous system and heart. When injecting cocaine, the drug goes directly into the bloodstream. This not only intensifies the euphoria, but also the health consequences.

Intradermal cocaine abuse is actually associated with Fournier’s gangrene. Further, “cocaine abuse is associated with a number of medical complications, most notably arrhythmias, myocardial infarction, and cerebral hemorrhage” (NLM).
Intradermally Injecting Opiates
Opiates like oxycodone, morphine, and heroin are the most commonly injected drugs and, like cocaine, they can lead to a lot of negative consequences. Opiates are classified as central nervous system depressants that cause a person to feel an intense euphoria, drowsiness, disorientation, and numbness. Heroin takes longer to reach the bloodstream through intradermal injection, so a person may use more of it to achieve a more intense high—increasing their chance of overdose.
Is Heroin More Addictive When Injected?
Some people believe that heroin isn’t as addictive when it’s snorted or used by skin-popping. This is not true. The drug is highly addictive no matter how it’s abused. The biggest difference between intravenous, intramuscular, intradermal, and nasal administration is the amount of time it takes for the substance to reach the brain.

According to the Center For Substance Abuse Research (CESAR), “intravenous injection provides the greatest intensity and most rapid onset of effects, as users can feel peak effects after 7 to 8 seconds. Intramuscular injection produces the euphoric high within 5 to 8 minutes, and when the drug is sniffed or smoked, effects are felt within 10 to 15 minutes.”
Heroin Overdose Statistics
CESAR goes on to describe the some of the side-effects of heroin by stating, “overdosing is a very real danger for heroin users. It is far more common than one might expect; a 2001 study in Australia concluded that 54% of regular injecting drug users reported experiencing at least one non-fatal overdose in their lifetime.”
Heroin overdose can include one or more of the following side effects:
- Extremely slow and shallow breathing
- Convulsions
- Pinpoint pupils
- Confusion
- Blue lips
- Weak pulse
- Low blood pressure
- Uncontrollable muscle spasms
- Disorientation
- Loss of consciousness
- Stopped breathing
- Coma
If someone is overdosing, they need to be taken to the hospital immediately. An overdose can be fatal.
Intramuscularly Injecting Anabolic Steroids
Anabolic steroids are the drugs most commonly abused by intramuscular injection, or muscling. Muscling occurs when a person injects a substance into the muscle instead of the vein, usually in the upper arms or legs. This method is commonly used in medicine for oral/dental surgeries, for substances that irritate the veins, or because a vein can’t be found. No matter which method is used for injecting, it can lead to abscesses, lesions, and tissue scarring.
Skin-Popping Abscesses, Lesions, And Scars
As substance abuse continues, the areas of injection become scarred, and lesions or abscesses start to form. When the body becomes infected, the immune system sends white blood cells to fight the infection. These injured sites become callused scar tissue over time.

“Scars are most commonly found on dorsal hands, digits, wrist, forearms, and lower extremities” (VisualDx). These scars and abscesses can last for life, and can show up years after a person stops.
Dangers And Complications Of Skin-Popping And Muscling
From Public Health Seattle And King County, “muscling and skin-popping allow germs to ‘sit’ inside muscle and fat tissue or under the skin. These are great places for abscesses and other infections to brew. Infections in these areas can be very serious. They can also spread to the blood, bones, heart and other places in the body. Some of the worst infections include wound botulism, tetanus (also called “lockjaw”) and necrotizing fasciitis (‘flesh eating disease’). If not treated quickly, these and other infections can become life-threatening and result in death.”
Treatment And Therapy For Addiction
Some people might continue abusing injectable substances to avoid painful withdrawal and intense cravings. Through a medically-supervised detoxification, these withdrawals and cravings can be managed through a healthy and natural process. After detox, addiction specialists, therapists, or psychologists can help patients better understand addiction, emotions, and behaviors.
Some of the most effective addiction treatment programs are:
- Professional Intervention
- Detoxification
- Evaluation
- Dialectical Behavior Therapy
- Cognitive Behavioral Therapy
- Mindfulness and Stress Management
- Contingency Management
- Individual and Group Therapy
- Healthy Living
- Peer Support Groups
- Family Therapy
- Aftercare Support
Finding The Right Treatment For You
If you or someone you love is struggling with addiction, we understand what you’re going through. We want to help you on your road to recovery. Contact us today to speak to one of our kind, caring professionals about skin-popping and rehab treatment.
For More Information Related to “The Dangers Of “Skin-Popping” Drugs” Be Sure To Check Out These Additional Resources From DrugRehab.org:
Sepsis From Intravenous (IV) Drug Use
Cellulitis From Intravenous (IV) Drug Use
Recovery Solutions: Hepatitis C Treatment For Former IV Drug Use
Understanding A Needle Fixation
Sources
Center For Substance Abuse Research—Heroin
Public Health Seattle And King County—Muscling and Skin Popping
U.S. National Library Of Medicine—Fournier’s gangrene associated with intradermal injection of cocaine
U.S. National Library Of Medicine—Pneumothorax: A Complication of ‘Skin Popping’
VisualDx—Skin Popping Substance Abuse



 Prescription drug abuse
Prescription drug abuse Even prescribed use of these drugs changes the way your CNS functions, earning them the term CNS
Even prescribed use of these drugs changes the way your CNS functions, earning them the term CNS 





 This is only a potential scenario, and doesn’t apply to everyone—the point is that though not everyone abuses prescription drugs for the same reason, all of our minds are wired the same way to crave things that make us feel good.
This is only a potential scenario, and doesn’t apply to everyone—the point is that though not everyone abuses prescription drugs for the same reason, all of our minds are wired the same way to crave things that make us feel good.

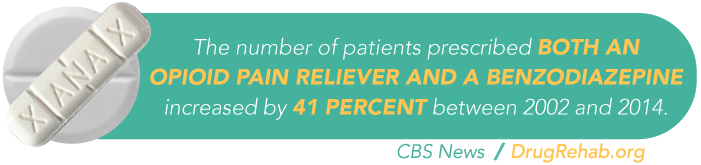
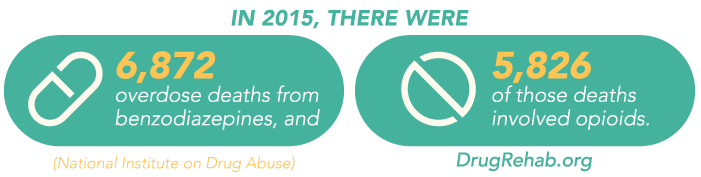
 Ativan is a brand name medication of the benzodiazepine (benzo) drug lorazepam. As a benzo, it’s a central nervous system (CNS) depressant, which means it slows several important bodily functions, including breathing rates, heart rate, and temperature. The
Ativan is a brand name medication of the benzodiazepine (benzo) drug lorazepam. As a benzo, it’s a central nervous system (CNS) depressant, which means it slows several important bodily functions, including breathing rates, heart rate, and temperature. The 
 Detox can be emotionally strenuous as well, which is another reason detoxing in a facility is so important. The facility’s staff will comfort you during this time, answering any questions you may have, or will simply provide an ear and any emotional support you may need.
Detox can be emotionally strenuous as well, which is another reason detoxing in a facility is so important. The facility’s staff will comfort you during this time, answering any questions you may have, or will simply provide an ear and any emotional support you may need.

 When used as a medical treatment, the prescribing doctor should gradually taper you off of the drug as to avoid unpleasant side effects of withdrawal. These professionals are trained and understand how to best do this to avoid any complications and further strain to your physical and mental states.
When used as a medical treatment, the prescribing doctor should gradually taper you off of the drug as to avoid unpleasant side effects of withdrawal. These professionals are trained and understand how to best do this to avoid any complications and further strain to your physical and mental states.
 Codeine has been mixed with different drugs to treat various medical conditions, most commonly acetaminophen. There are various strengths of this drug combination, indicated in the title of the drug as Tylenol 2, Tylenol 3, and Tylenol 4. Tylenol 4 is the most potent of these medications, containing 60mg of codeine and 325mg of acetaminophen.
Codeine has been mixed with different drugs to treat various medical conditions, most commonly acetaminophen. There are various strengths of this drug combination, indicated in the title of the drug as Tylenol 2, Tylenol 3, and Tylenol 4. Tylenol 4 is the most potent of these medications, containing 60mg of codeine and 325mg of acetaminophen. While reducing the amount and frequency of opioids if you have a substance abuse issue is important, quitting abruptly can be extremely dangerous. Because your brain has become accustomed to a certain level of opioids binding with your opioid receptors, your body considers this new chemical balance to be the norm. If you suddenly stop taking opioids, then this level will come down too rapidly, resulting in withdrawal symptoms.
While reducing the amount and frequency of opioids if you have a substance abuse issue is important, quitting abruptly can be extremely dangerous. Because your brain has become accustomed to a certain level of opioids binding with your opioid receptors, your body considers this new chemical balance to be the norm. If you suddenly stop taking opioids, then this level will come down too rapidly, resulting in withdrawal symptoms.
 Suboxone is a fairly new drug to the addiction treatment market. Intended to treat all types of opioid addiction in adults, Suboxone is actually a combination of two different types of drugs; buprenorphine and naloxone. Often prescribed for pain control,
Suboxone is a fairly new drug to the addiction treatment market. Intended to treat all types of opioid addiction in adults, Suboxone is actually a combination of two different types of drugs; buprenorphine and naloxone. Often prescribed for pain control, 
 With this tolerance generally comes increased or more frequent consumption of the drug, which can lead to serious long-term effects down the road. These
With this tolerance generally comes increased or more frequent consumption of the drug, which can lead to serious long-term effects down the road. These 
 Temazepam is one of the many sedatives that can be used to help a person sleep, but in the illicit market, there’s a lot of room for diversion and abuse of it. Perhaps you’ve never heard of it, but temazepam a much bigger problem than most of us realize.
Temazepam is one of the many sedatives that can be used to help a person sleep, but in the illicit market, there’s a lot of room for diversion and abuse of it. Perhaps you’ve never heard of it, but temazepam a much bigger problem than most of us realize. Temazepam and other benzodiazepines are classified as schedule IV depressants by the
Temazepam and other benzodiazepines are classified as schedule IV depressants by the  During this time, you’ll gradually be taken off the benzodiazepine, and your withdrawal symptoms will be carefully monitored by professionals.
During this time, you’ll gradually be taken off the benzodiazepine, and your withdrawal symptoms will be carefully monitored by professionals.







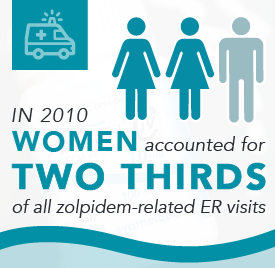
 Overall, benzodiazepine use was almost twice as prevalent in women as it was in men. This could be due to a wider social acceptance of women speaking with a psychiatrist about emotional issues than men, however it could also be linked to other environmental factors.
Overall, benzodiazepine use was almost twice as prevalent in women as it was in men. This could be due to a wider social acceptance of women speaking with a psychiatrist about emotional issues than men, however it could also be linked to other environmental factors.
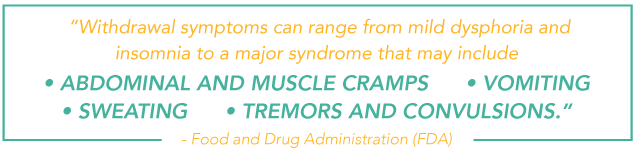
 The FDA sums it up perfectly, “abuse is characterized by misuse of the drug for nonmedical purposes, often in combination with other psychoactive substances. Physical dependence is a state of adaptation that is manifested by a specific withdrawal syndrome that can be produced by abrupt cessation, rapid dose reduction, decreasing blood level of the drug and/or administration of an antagonist…Tolerance is a state of adaptation in which exposure to a drug induces changes that result in a diminution of one or more of the drug’s effects over time.”
The FDA sums it up perfectly, “abuse is characterized by misuse of the drug for nonmedical purposes, often in combination with other psychoactive substances. Physical dependence is a state of adaptation that is manifested by a specific withdrawal syndrome that can be produced by abrupt cessation, rapid dose reduction, decreasing blood level of the drug and/or administration of an antagonist…Tolerance is a state of adaptation in which exposure to a drug induces changes that result in a diminution of one or more of the drug’s effects over time.”