The body has a process for breaking down alcohol. The amount of time alcohol stays in a person’s body depends on how much they drink and their overall health. After prolonged alcohol use, the liver, brain, and other organs may suffer great damage.
Understanding The Effects Of Alcohol
Alcohol (ethanol) is a central nervous system depressant that spends relatively little time in the body, but causes its functions to slow. The amount of time alcohol spends in a person’s body depends greatly on the size of their liver and their body mass. On average, the body metabolizes alcohol at a constant rate of 20 milligrams per deciliter (mg/dL) per hour.
“Alcohol slows your breathing rate, heart rate, and how well your brain functions. These effects may appear within 10 minutes and peak at around 40 to 60 minutes. Alcohol stays in your bloodstream until it is broken down by the liver,” (National Library of Medicine).

Alcohol affects each person differently. A person’s blood alcohol concentration (BAC) is determined by environmental factors such as amount consumed, presence of food in the system, type of alcoholic beverage, and genetic factors. Two people can drink the same amount of alcohol, and it will have a different effect on each of them, and different effects on their BAC.
Factors that can affect how a person’s body reacts to alcohol include:
- age
- weight
- gender
- physical health
- genetics
- smoking
- how much and how often a person drinks
- mixing alcohol with medications or other drugs
- drinking a large amount of alcohol in a short period of time (binge drinking)
Many people drink alcohol as a way to unwind or socialize. Yet too much alcohol can damage the liver, heart, stomach, pancreas, and immune system. Abusing alcohol, binge drinking, or using alcohol to try to cope with grief, anxiety, depression, or mental illness, may contribute to alcohol use disorder.
Are you or a loved one suffering from addiction?
Don't wait, get the best treatment options today
Call Now: (833) 473-4227What Is Alcohol Use Disorder?
Alcohol use disorder (AUD) is a condition that occurs when the use of alcohol causes significant impairment, health problems, or distress. Many people suffering from AUD become unable to meet requirements with their career, school, or home life.
Alcohol use disorder is a progressive and primary illness. If left untreated, AUD will continue to get worse over time as drinking progresses. AUD is defined as mild, moderate, or severe.
How Is Alcohol Metabolized?
After alcohol is consumed, it quickly travels to the digestive system. The stomach tissues absorb about 20 percent of the alcohol into the bloodstream, which is known as gastric emptying. The other 80 percent of alcohol is absorbed into the tissues of the small intestine.
First-pass metabolism (FPM) is greatly influenced by the speed of gastric emptying, which can also vary based on the amount of food in a person’s system, how much they drank, their age, and their overall physical health.
Once alcohol has been absorbed into the bloodstream, it travels through the veins to the liver, where it’s exposed to enzymes and metabolized. The principle alcohol-metabolizing enzymes within the liver include alcohol dehydrogenase (ADH) and aldehyde dehydrogenase (ALDH).
ADH metabolizes alcohol to acetaldehyde, which is a highly toxic substance that may contribute to organ tissue damage and alcohol addiction. After that, acetaldehyde is broken down into acetate, which is then oxidized into carbon dioxide in the heart, skeletal muscles, and brain cells.
Researchers have found that a person’s genetics can be a factor in the amount of ADH and ALDH enzymes they have in their body. People have different variations of ADH and ALDH enzymes in their body, and some people are able to process alcohol faster than others.
Liver Metabolism Rates
The liver is responsible for the final step of removing alcohol from the body, but any issues with the liver can slow this process. On average, it takes the liver one hour to metabolize one ounce of alcohol. The liver is the primary organ responsible for metabolizing ingested ethanol, but non-liver tissues, like the brain, can metabolize alcohol as well.
For many people, an ounce of alcohol produces a .015 blood alcohol concentration (BAC). The more alcohol a person drinks, the higher their BAC becomes. In other words, the amount of time it takes the liver to process alcohol is greatly affected by the amount a person drinks.
A person who suffers from an alcohol use disorder may not be able to control the amount they drink, which not only increases their chance of acute alcohol intoxication, but also increases the chance of doing serious damage to the liver and other organs.
Alcohol’s Effect On The Body
Even though its time in the body is considerably short compared to many other drugs, alcohol can have a serious impact on a person’s health on any single occasion or over time. The rate at which the the body metabolizes alcohol is greatly affected by organ health. Alcohol can cause damage to the heart, liver, brain, pancreas, and contributes to certain cancers as well.
- Brain—Alcohol slows communication speed between neurotransmitters in the brain. Alcohol also shrinks brain cells and damages the cerebellum, limbic system, and cerebral cortex. Abstinence from alcohol can help reverse negative effects on problem-solving skills, memory, and attention.
- Liver—Heavy alcohol consumption takes a serious toll on the liver, and can lead to a number of liver problems and liver inflammation. Liver problems caused by alcohol include fatty liver, alcoholic hepatitis, fibrosis, and cirrhosis.
- Heart—Some of the heart problems from alcohol include alcoholic cardiomyopathy, arrhythmia, stroke, and high blood pressure. Long-term heavy drinking is a leading cause of heart disease, which kills an estimated 610,000 people each year.
- Pancreas—Alcohol causes the pancreas to produce a toxic substance which can lead to pancreatitis. Pancreatitis is a dangerous swelling of the blood vessels in the pancreas that prevents proper digestion.
- Cancer—Heavy drinking increases the risk of developing cancers, which may include mouth cancer, esophagus cancer, throat cancer, breast cancer, and liver cancer.
Alcohol damage to any single organ may cause a chain reaction of organ damage. According to the National Institute on Alcohol Abuse and Alcoholism, “The liver breaks down alcohol—and the toxins it releases. During this process, alcohol’s byproducts damage liver cells. These damaged liver cells no longer function as well as they should and allow too much of these toxic substances, ammonia and manganese in particular, to travel to the brain.”
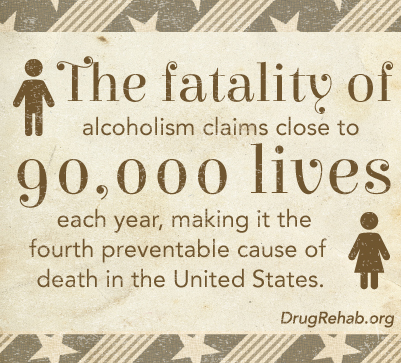
Alcohol doesn’t just damage the body. With too much alcohol, a person can develop alcohol dependence (alcoholism), loss of job, mental disorder, and even die. Alcohol poisoning is responsible for six deaths every day in the United States.
How To Detoxify Your Body From Alcohol
A medically-supervised detoxification (medical detox) takes place at a residential treatment center, and is performed by a team of physicians, clinicians, nurses, and treatment professionals. Medical detox helps patients through potential withdrawal symptoms and other complications found in early abstinence from alcohol. Medical detox is the safest and most effective way to remove alcohol from the body.
Medical detox is an initial step toward recovering from alcohol, but isn’t considered a full treatment. Addiction is a progressive illness, which means that it doesn’t go away over time, but gets worse. Quitting alcohol may help an individual avoid serious health risks.
Contact DrugRehab.org for help with quitting use of alcohol.
For More Information Related to “How Long Does Alcohol Stay In Your Body?” Be Sure To Check Out These Additional Resources From DrugRehab.org:















 Alcohol is a small molecule that interacts with a lot of different neurotransmitters in the brain, including: GABA, endorphins, dopamine, norepinephrine, glutamate, and adrenaline. Alcohol causes dependency, partly because as a person drinks, the dopamine in the reward pathway of the brain is increased.
Alcohol is a small molecule that interacts with a lot of different neurotransmitters in the brain, including: GABA, endorphins, dopamine, norepinephrine, glutamate, and adrenaline. Alcohol causes dependency, partly because as a person drinks, the dopamine in the reward pathway of the brain is increased. There are three stages to alcohol withdrawal, the first of which can begin as early 6 hours after a person’s peak intoxication. The stages go from mild to moderate to severe, and can last anywhere from 5 to 7 days. Generally after a week, the majority of withdrawal symptoms will have subsided, however, some may persist for several weeks without proper treatment.
There are three stages to alcohol withdrawal, the first of which can begin as early 6 hours after a person’s peak intoxication. The stages go from mild to moderate to severe, and can last anywhere from 5 to 7 days. Generally after a week, the majority of withdrawal symptoms will have subsided, however, some may persist for several weeks without proper treatment.





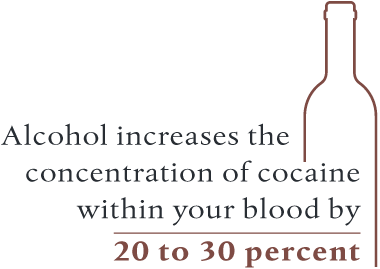 For individuals who aren’t accustomed to consuming alcohol with crack, the potential for a fatal overdose skyrockets. Alcohol can actually make it easier for your body to absorb cocaine, which increases the concentration of cocaine within your blood by 20 to 30 percent. From this effect, a person could overdose if they take an amount they are typically used to when using the drug alone.
For individuals who aren’t accustomed to consuming alcohol with crack, the potential for a fatal overdose skyrockets. Alcohol can actually make it easier for your body to absorb cocaine, which increases the concentration of cocaine within your blood by 20 to 30 percent. From this effect, a person could overdose if they take an amount they are typically used to when using the drug alone.
 Alcohol abuse
Alcohol abuse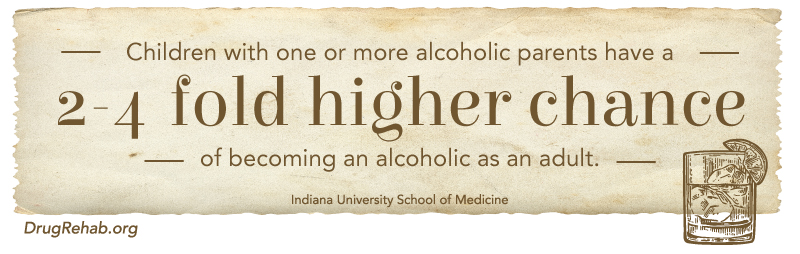
 Alcohol withdrawals
Alcohol withdrawals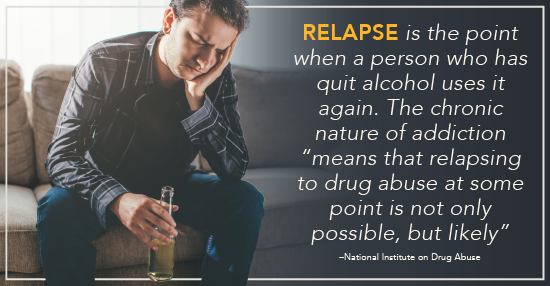
 In summary, alcohol withdrawal is not only a result of a physical demand of the chemical, but also the cognitive function in trying to maintain normal function.
In summary, alcohol withdrawal is not only a result of a physical demand of the chemical, but also the cognitive function in trying to maintain normal function.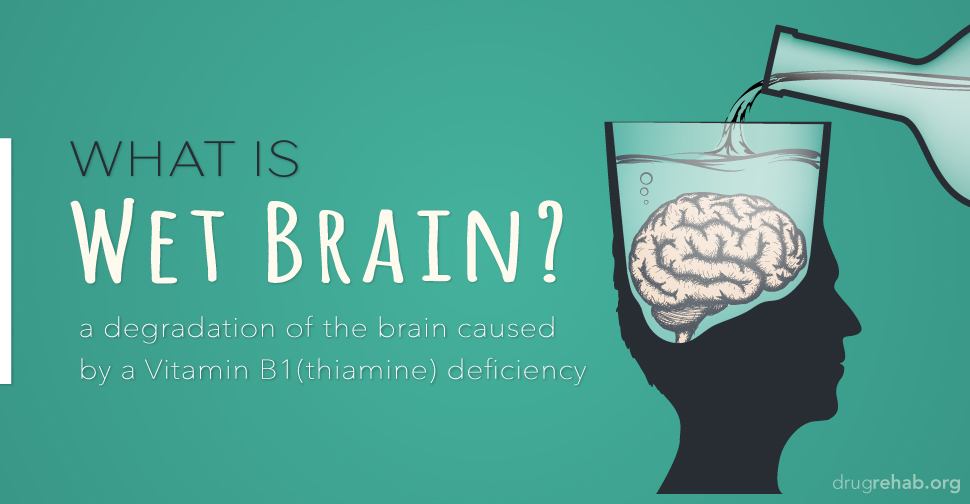


 If you suspect a friend or family member is abusing alcohol, it is important to look closely for the signs related to alcohol abuse. Keep in mind this is much more about their behavior surrounding the consumption of alcohol, and not necessarily limited to the amount of alcohol they consume.
If you suspect a friend or family member is abusing alcohol, it is important to look closely for the signs related to alcohol abuse. Keep in mind this is much more about their behavior surrounding the consumption of alcohol, and not necessarily limited to the amount of alcohol they consume.