Methamphetamine abuse can lead to binges which last several days. Abuse of meth, especially prolonged abuse, can be damaging to a person’s health. Binges can result in irritability, paranoia, and even psychosis. Knowing how long methamphetamine stays in your system can be useful when meth abuse is suspected. Methamphetamine abuse and addiction are best treated under careful monitoring in an inpatient environment.
Methamphetamine, commonly called meth, produces an instant, though short-lived, rush feeling for those who take it. It’s the reason many seek the drug. But because the rush wears off quickly, many people seek meth again and again.
Drugs which produce an initial rush followed by a high (feeling of intense euphoria and increased activity) tend to be highly addictive. Meth is no exception. Yet the stages of meth abuse can be dangerous, especially for those who continually abuse the drug.
It may be helpful to know how long methamphetamine stays in your system if you believe someone you know is abusing the drug. Meth abuse leads to a number of risks, including dissociation of the mind and high risk of self-harm or harm to others (at worst). Treatment is the safest way to ensure those abusing meth find help to quit use of it.
Duration Of Meth In Your System
Research conducted on how long meth stays in the body often involves the blood-to-plasma ratio. This measures the amount of meth in the whole blood. Other measurements may examine only how much meth is in plasma, which can be misleading if concentrations of the drug differ between red blood cells and plasma.
Measures of meth in your system works like this, according to the National Highway Traffic Safety Administration (NHTSA):
- Peak blood methamphetamine concentrations:
- A few minutes after smoking or injecting
- Around 3 hours after taking orally
- Peak amphetamine concentrations (after broken down from methamphetamine):
- 12 hours
- Elimination half-life (time to meth concentration cut in half):
- Mean measure is 10.1 hours
- Range of 6.4 to 15 hours
For each dose of meth, it takes anywhere from two to 10 days to leave the body. This number can change though, depending on usage; the more meth abused, the longer it takes to leave the body.

The short-term side effects experienced can last up to 24 hours, but with binges, this can change. Detection of meth in drug tests is confirmed usually within one to four days after use, but can be confirmed up to a week after heavy use, according to the NHTSA.
The Stages Of The Meth High
- Initial rush:
- When a person abuses meth, he or she first experiences the rush, or the initial surge of euphoria. This feeling lasts from a few minutes up to 30 minutes.
- During that time, the person’s heart rate increases and other systems in the body escalate, including blood pressure, pulse, and metabolism.
- High:
- After the rush comes the high. According to DrugFreeWorld.org, “during the high the abuser often feels aggressively smarter and becomes argumentative, often interrupting other people and finishing their sentences.” This stage is often characterized by delusions.
- Delusions lead the person to focus solely on one small thing; the person may place high importance on small tasks, like repetitive motions (stroking something or wiping a surface). The high can last from four to 16 hours.
- Binge:
- People affected by meth abuse may take several doses in a row to ensure a string of continuous highs. This process, known as a binge, results in hyperactivity. When a person abusing meth goes on a binge, he or she can go for days without sleep or food.
- Binges can last three to up to 15 days, according to the Center for Abuse Substance Research (CESAR). The purpose of the binge is to continue the high and re-experience the rush. But each time a person injects or smokes meth, the rush is less potent, the high less effective, until neither is experienced at all.
- Tweaking:
- It is during the binge that a person abusing meth experiences the most dangerous stage of meth abuse: tweaking. After lack of sleep and food for days, and with a constant stream of meth in the system, a person becomes paranoid and irritable.
- Though this stage is plagued by intense craving for the rush and high, the person likely can’t get the desired effects because he or she has developed tolerance.
- Tweaking presents danger because it may result in violence which can lead to domestic disputes or criminal acts, or even car accidents.
- Tweaking is characterized by: eyes moving extremely fast, quivering voice, jerky movements.
Factors For Duration
Because many people who abuse meth engage in a binge, it is important to know how long meth stays in your system. A few things affect the duration of meth in the body, and include:
- Method of administration: smoked, injected, or swallowed. Smoking or injecting results in quick onset; taking orally results in slower onset.
- How many doses have been taken
- How long it has been since last dose
- How well it is metabolized: the state of your liver and kidneys
How Is Meth Metabolized?
The body immediately begins to metabolize meth, first breaking it down partly to amphetamine. Within a few hours, the body continues to break down the methamphetamine and amphetamine left in the bloodstream.
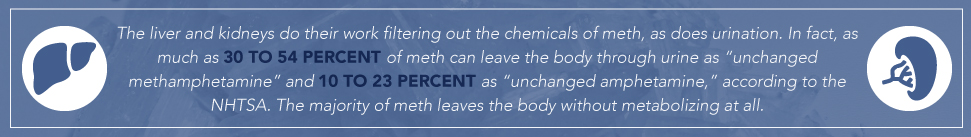
The liver and kidneys do their work filtering out the chemicals of meth, as does urination. In fact, as much as 30 to 54 percent of meth can leave the body through urine as “unchanged methamphetamine” and 10 to 23 percent as “unchanged amphetamine,” according to the NHTSA. The majority of meth leaves the body without metabolizing at all.
How Does Meth Affect Your Health?
In addition to being highly addictive, meth can cause damaging effects to your health. Psychological dependence can result because the rush effects are desirable: excitement, high energy, talkativeness. People who abuse meth may associate this time with increased abilities to perform or achieve tasks (part of the delusions they experience).
But taking high doses or prolonged abuse can lead to less desirable effects to your health. For example, chronic use can lead to: irritability, nervousness, paranoia, violent behavior and extreme depression. All of these symptoms can contribute to increased likelihood of self-harm or harm of others. Left untreated, prolonged meth abuse can trigger psychosis similar to schizophrenia.
Adverse health effects associated with long-term abuse may include:
- Meth mouth: tooth decay, cracked teeth, and gum disease
- Brain damage
- Breakdown of immune system
- Skin lesions (sores)
- High blood pressure
- Extreme weight loss
- Malnutrition
- Stroke
- Heart problems
- Lung disease
- Kidney or liver damage
- Overdose and death
How Do You Treat Methamphetamine Abuse?
Treatment for meth first involves detoxification (detox). This first necessary step allows chemicals acquired during abuse to leave the body. This process can be dangerous when performed alone. Inpatient rehab centers can provide the medical and professional support necessary to get through it.
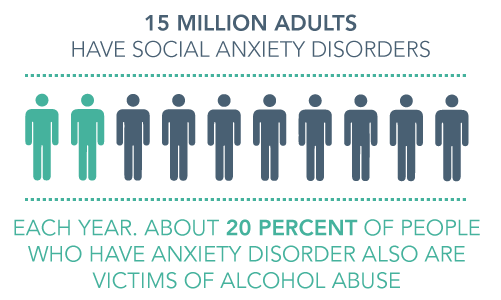
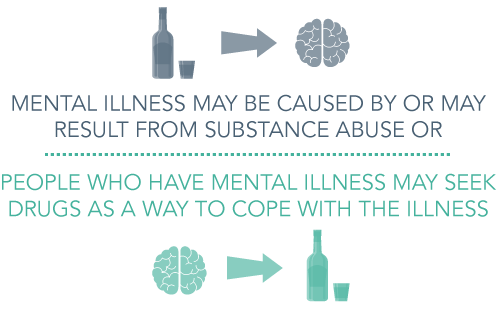
After being assessed, you’ll get treatment for meth abuse and any co-occurring substance abuse disorders or mental health disorders. Meth abuse may be coupled with alcohol abuse or abuse of other depressants, and can be characterized by anxiety, depression, or psychosis. It is important to recognize and treat all co-occurring disorders to ensure the best chance at recovery.
Inpatient rehab centers can provide the mental and emotional support you’ll lack in outpatient treatment. Evidence-based treatment options and licensed medical staff make treatment in a rehab center the quality experience it should be—a chance to rebuild a life without meth.
Get Information About Treatment
When people we know are in the grips of addiction, it can be frightening. Methamphetamine binges can last for days, and if someone you know is experiencing this, you may not know what to do next. We can help get your loved one into treatment, and find a recovery plan that works. Contact us today at DrugRehab.org to learn more about treating meth addiction and the rehab center difference.
For More Information Related to “How Long Does Methamphetamine Stay In Your System?” Be Sure To Check Out These Additional Resources From DrugRehab.org:
- Meth Drug Rehab
- Signs Of Methamphetamine Psychosis
- How Do I Get My Loved One Into Rehab?
- A New Weapon in The Meth Crisis
- The Effects of Drugs and Alcohol on the Kidneys
Sources
Center For Abuse Substance Research—Methamphetamine
Drug Free World—The Stages Of The Meth Experience
National Highway Traffic Safety Administration—Methamphetamine (And Amphetamine)
National Institute On Drug Abuse—DrugFacts: Methamphetamine
National Institute On Drug Abuse—What Are The Long-Term Effects Of Methamphetamine Abuse?





 Every little kid walks through a dark alley and gets the heebie jeebies, it’s just part of growing up. As they get older and recognize that there is no boogie man there to get them, they relinquish the fear and grow out of it. Some people go through life with that constant fear that something bad will happen. They very well could be suffering from a panic attack, which is defined by the
Every little kid walks through a dark alley and gets the heebie jeebies, it’s just part of growing up. As they get older and recognize that there is no boogie man there to get them, they relinquish the fear and grow out of it. Some people go through life with that constant fear that something bad will happen. They very well could be suffering from a panic attack, which is defined by the 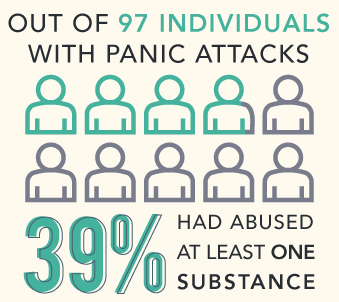 Not every substance will cause a panic attack, however, there are certain drugs that can. Some people suffering from a
Not every substance will cause a panic attack, however, there are certain drugs that can. Some people suffering from a  Caffeine is not always associated with substance abuse; however, it’s still a drug. When caffeine is consumed in heavy quantities, or more than a healthy amount, that’s abuse. Caffeine is a stimulant, and after it’s ingested (whether it’s in a pill form or in a beverage) it raises the heart rate. According to the
Caffeine is not always associated with substance abuse; however, it’s still a drug. When caffeine is consumed in heavy quantities, or more than a healthy amount, that’s abuse. Caffeine is a stimulant, and after it’s ingested (whether it’s in a pill form or in a beverage) it raises the heart rate. According to the  Alcohol is a drug which is sometimes referred to as “liquid courage”, because it can cause a person to do things that they might not normally do. Alcohol can lead to mood swings and temper tantrums–a person who abuses alcohol may exhibit bouts of rage, anxiety, and increased danger to his or herself and others. Withdrawal from alcohol can also lead to symptoms such as anxiety and panic attacks, but it can also lead to insomnia, delirium tremens, sweating profusely,
Alcohol is a drug which is sometimes referred to as “liquid courage”, because it can cause a person to do things that they might not normally do. Alcohol can lead to mood swings and temper tantrums–a person who abuses alcohol may exhibit bouts of rage, anxiety, and increased danger to his or herself and others. Withdrawal from alcohol can also lead to symptoms such as anxiety and panic attacks, but it can also lead to insomnia, delirium tremens, sweating profusely,  Marijuana can be smoked, consumed, or “dabbed”–the highest dose of tetrahydrocannabinol THC which can be abused. THC is the primary compound found in marijuana, and it can have serious affects on the mind of a person using it. Abuse of marijuana can lead to lack of motivation, mood swings, anxiety, and panic attacks. The
Marijuana can be smoked, consumed, or “dabbed”–the highest dose of tetrahydrocannabinol THC which can be abused. THC is the primary compound found in marijuana, and it can have serious affects on the mind of a person using it. Abuse of marijuana can lead to lack of motivation, mood swings, anxiety, and panic attacks. The 
 Opioids such as heroin are characterized by spurts of intense euphoria and well-being. Abusing drugs like heroin can lead to anxiety, severe depression, and insomnia. Even after a person stops using opioids, the withdrawals can start after a couple hours and last for several weeks–withdrawal symptoms can be incredibly dangerous and sometimes include paranoia, anxiety, panic, and seizures. With the prolonged withdrawals associated with opioids, relapse is more likely to occur to avoid further withdrawals.
Opioids such as heroin are characterized by spurts of intense euphoria and well-being. Abusing drugs like heroin can lead to anxiety, severe depression, and insomnia. Even after a person stops using opioids, the withdrawals can start after a couple hours and last for several weeks–withdrawal symptoms can be incredibly dangerous and sometimes include paranoia, anxiety, panic, and seizures. With the prolonged withdrawals associated with opioids, relapse is more likely to occur to avoid further withdrawals. Hallucinogens can give the user visual and mental delusions–or hallucinations. A person who is abusing hallucinogens (such as LSD, Peyote, PCP, and Psilocybin Mushrooms (or Shrooms)) can become dangerously antisocial. They might experience bouts of laughter, which can be followed by unexplainable crying. A person using these kind of drugs can very quickly slip into a drug induced panic attack, or lapse into paranoia. Withdrawal from some hallucinogens can be feeling of emptiness, prolonged trip (or “permi-trip”), inability to eat, anxiety, and fatigue.
Hallucinogens can give the user visual and mental delusions–or hallucinations. A person who is abusing hallucinogens (such as LSD, Peyote, PCP, and Psilocybin Mushrooms (or Shrooms)) can become dangerously antisocial. They might experience bouts of laughter, which can be followed by unexplainable crying. A person using these kind of drugs can very quickly slip into a drug induced panic attack, or lapse into paranoia. Withdrawal from some hallucinogens can be feeling of emptiness, prolonged trip (or “permi-trip”), inability to eat, anxiety, and fatigue.
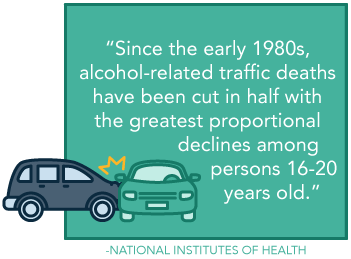 Despite its legal standing, prevalence, and acceptance within numerous social spheres, alcohol is not a benign drug. One of the most common and destructive ways in which this occurs is within circumstances regarding an individual driving after they have been drinking. In decades past, this behavior was more commonplace and even somewhat socially acceptable. Fortunately now, with the advent of more strident rules and social perspectives, this behavior has declined, as evidenced, in part, by statistics presented by the
Despite its legal standing, prevalence, and acceptance within numerous social spheres, alcohol is not a benign drug. One of the most common and destructive ways in which this occurs is within circumstances regarding an individual driving after they have been drinking. In decades past, this behavior was more commonplace and even somewhat socially acceptable. Fortunately now, with the advent of more strident rules and social perspectives, this behavior has declined, as evidenced, in part, by statistics presented by the 
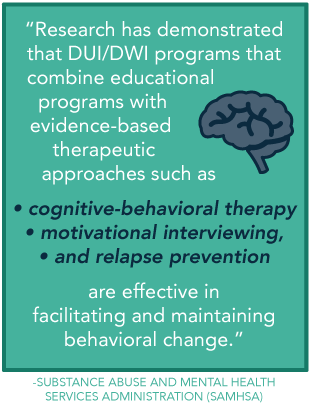 Yes. While you will likely be able to choose most any program, there are certain programs that are especially designed for DUI/DWI offenders. According to the Substance Abuse and Mental Health Services Administration (SAMHSA) “
Yes. While you will likely be able to choose most any program, there are certain programs that are especially designed for DUI/DWI offenders. According to the Substance Abuse and Mental Health Services Administration (SAMHSA) “
 Narcissism is rarely a desired attribute, though it is often directly related to a personality disorder. Personality disorders fall into the
Narcissism is rarely a desired attribute, though it is often directly related to a personality disorder. Personality disorders fall into the 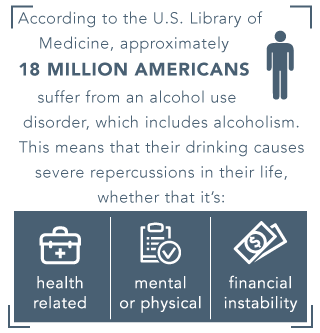 According to the
According to the  A person who is suffering from alcoholism and narcissistic personality disorder, might answer the question (How the heck aren’t you drunk yet?), with a false sense of pride or by stating anything other than “because I can’t stop drinking”, or by stating, “I have built up a tolerance.” There are many accomplishments that deserve a person the right to be proud of themselves, but unfortunately, alcoholism is not one of them, and it’s dangerous to believe that it is. Intervention and treatment are very likely the only way to get a person on the right track towards recovery. Try to remember that Alcoholism is a disease and the person with it is very sick.
A person who is suffering from alcoholism and narcissistic personality disorder, might answer the question (How the heck aren’t you drunk yet?), with a false sense of pride or by stating anything other than “because I can’t stop drinking”, or by stating, “I have built up a tolerance.” There are many accomplishments that deserve a person the right to be proud of themselves, but unfortunately, alcoholism is not one of them, and it’s dangerous to believe that it is. Intervention and treatment are very likely the only way to get a person on the right track towards recovery. Try to remember that Alcoholism is a disease and the person with it is very sick.
 Autism is much more common today than it was in past decades. The current number of children affected by autism is a ten-fold increase from forty years ago, according to Psychology Today. Research suggests autism gets its start in early brain development; one of the suggested ways to prevent autism for pregnant mothers is a diet high in folic acid. However, autism may be diagnosed in children two to three years of age—when symptoms tend to become obvious. Autism is also more common in boys than in girls.
Autism is much more common today than it was in past decades. The current number of children affected by autism is a ten-fold increase from forty years ago, according to Psychology Today. Research suggests autism gets its start in early brain development; one of the suggested ways to prevent autism for pregnant mothers is a diet high in folic acid. However, autism may be diagnosed in children two to three years of age—when symptoms tend to become obvious. Autism is also more common in boys than in girls. Autism is not typically associated with alcohol or drug abuse. Psychology Today explains that people with autism are traditionally not drawn to alcohol abuse because they tend to have a “preference for low risk and avoidance of social situations.” But the newest findings point to a heightened risk of addiction for those with autism. When two disorders occur together, they are called
Autism is not typically associated with alcohol or drug abuse. Psychology Today explains that people with autism are traditionally not drawn to alcohol abuse because they tend to have a “preference for low risk and avoidance of social situations.” But the newest findings point to a heightened risk of addiction for those with autism. When two disorders occur together, they are called  The goal for those with autism is often to move them into a manageable state of the disorder, and some reach this level. For those who don’t, and who develop addiction to drugs or alcohol, treatment is the best help available.
The goal for those with autism is often to move them into a manageable state of the disorder, and some reach this level. For those who don’t, and who develop addiction to drugs or alcohol, treatment is the best help available. 
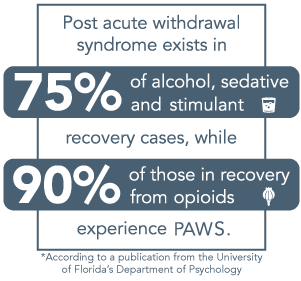 Like acute withdrawal, this collection of symptoms may push a person towards thoughts of returning to drug or alcohol use, in an attempt to squash the symptoms. Because of this, it is extremely important that a person, and their family members, be aware of PAWS and its symptoms, should it arise, as it is far more prevalent than you may think. The reality is, according to a
Like acute withdrawal, this collection of symptoms may push a person towards thoughts of returning to drug or alcohol use, in an attempt to squash the symptoms. Because of this, it is extremely important that a person, and their family members, be aware of PAWS and its symptoms, should it arise, as it is far more prevalent than you may think. The reality is, according to a 
 When confronted with symptoms of PAWS, your physician or other treatment provider will take several steps to ascertain the situation, to ensure an accurate diagnosis and full treatment. Post acute withdrawal syndrome shares a variety of symptoms with other conditions, including various co-occurring disorders. For this reason, your care provider should assess, and reassess as necessary, for any accompanying disorders such as depression. In some circumstances, a person may have both PAWS and a co-occurring disorder. Addressing treatment needs of the dual diagnosis condition will help a person to more effectively recover and help to prevent relapse. At this time, they will also likely address any sleep problems, while ruling out other medical conditions.
When confronted with symptoms of PAWS, your physician or other treatment provider will take several steps to ascertain the situation, to ensure an accurate diagnosis and full treatment. Post acute withdrawal syndrome shares a variety of symptoms with other conditions, including various co-occurring disorders. For this reason, your care provider should assess, and reassess as necessary, for any accompanying disorders such as depression. In some circumstances, a person may have both PAWS and a co-occurring disorder. Addressing treatment needs of the dual diagnosis condition will help a person to more effectively recover and help to prevent relapse. At this time, they will also likely address any sleep problems, while ruling out other medical conditions.
 One of the biggest changes between the DSM-IV and DSM-V criteria, is the
One of the biggest changes between the DSM-IV and DSM-V criteria, is the 

 Feelings of sadness
Feelings of sadness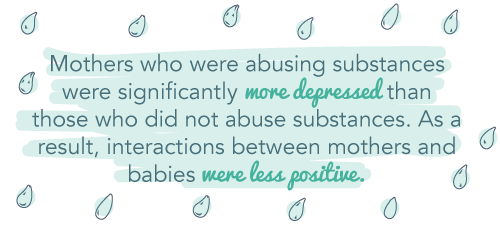
 Some types of treatment for postpartum depression include antidepressants and psychotherapy, the
Some types of treatment for postpartum depression include antidepressants and psychotherapy, the 
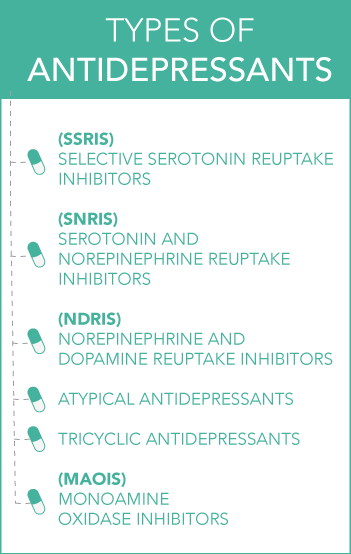 As each person and their circumstances, level of depression, and physiology are different, there are various medications within the antidepressant class. They include:
As each person and their circumstances, level of depression, and physiology are different, there are various medications within the antidepressant class. They include: Though it is of yet controversial whether or not a person can be addicted to antidepressants, and in turn experience a tolerance or compulsive desire to use, a person may develop aberrant behaviors surrounding their drug use. If you see any of the following, it may point to this problem:
Though it is of yet controversial whether or not a person can be addicted to antidepressants, and in turn experience a tolerance or compulsive desire to use, a person may develop aberrant behaviors surrounding their drug use. If you see any of the following, it may point to this problem: Though research is mixed, some findings suggest that SSRIs may actually be linked to
Though research is mixed, some findings suggest that SSRIs may actually be linked to 
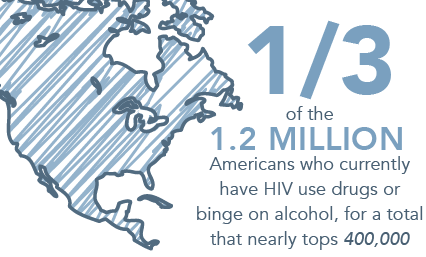
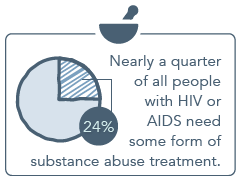 Treating HIV or AIDS and drug addiction at the same time is often complicated by a variety of concerns. Beyond the health problems that both cause (such as low energy, malnutrition, and susceptibility to outside diseases), lies the fact that many HIV/AIDS medications may actually cause multiple side effects that makes drug addiction more difficult to physically handle.
Treating HIV or AIDS and drug addiction at the same time is often complicated by a variety of concerns. Beyond the health problems that both cause (such as low energy, malnutrition, and susceptibility to outside diseases), lies the fact that many HIV/AIDS medications may actually cause multiple side effects that makes drug addiction more difficult to physically handle. for facing current or future relationships and to decrease their chance of transmitting HIV.
for facing current or future relationships and to decrease their chance of transmitting HIV.