In 2014, there were an estimated 1.5 million people using cocaine in the United States, but finding out if your loved one is using cocaine can be tricky, especially if you don’t know what to look for.
Cocaine is a white powder that people can snort up their nose, or mix with liquid then inject into their bloodstream. Cocaine’s dangerous. It’s a central nervous system stimulant that overstimulates the brain’s reward circuit. Cocaine can increase a person’s heart rate to an alarming level.
There are several signs that may give you a better idea, if you believe that someone is using cocaine. It’s important to know what to look for, because your loved one might need help quitting cocaine. Many people find freedom from cocaine in the safety of a rehab center.
1. Lack Of Money From Cocaine Use
 One of the first signs of cocaine use will appear when an individual runs out of money. Cocaine is one of the more expensive drugs, and the high from it doesn’t last very long so one binge can be costly. According to the National Institute on Drug Abuse (NIDA), “snorting cocaine produces a relatively slow onset of the high, but it may last from 15 to 30 minutes.”
One of the first signs of cocaine use will appear when an individual runs out of money. Cocaine is one of the more expensive drugs, and the high from it doesn’t last very long so one binge can be costly. According to the National Institute on Drug Abuse (NIDA), “snorting cocaine produces a relatively slow onset of the high, but it may last from 15 to 30 minutes.”
A cocaine binge can cost 150 dollars per gram, and can last for several days, weeks, or months. Some people spend so much on cocaine that they’re unable to support themselves, or their family on an otherwise substantial income. Cocaine use has been known to ruin lives, and may even cost a person their job. In this respect, a person abusing cocaine may constantly need to borrow money, whether they have a job or not.
2. Drug Paraphernalia Used For Cocaine
Another sign of cocaine abuse is the appearance of drug paraphernalia, which refers to objects, and miscellaneous articles needed to use the drug. Here’s a list of paraphernalia used for cocaine:
- Tightly rolled dollar bills
- Straws
- Tubes
- Pens with the ends cut off
- Sandwich baggies
- Flat surface with white residue:
- Piece of glass
- Mirror
- Tray
- Book
- Countertop
- Magazine
- Burnt spoons
- Unexplained needles or syringes
- Glass pipe
- Concealable containers with white residue
Some of these items won’t show up, because your loved one may keep it well hidden, or clean up after using the drug. It can also depend on when and where an individual uses cocaine. If you decide to confront someone about their cocaine use, they might not be honest with you—at least not at first. It may be helpful to have them take a random at home drug test, if you suspect your loved one is using cocaine.
3. Behavioral Changes From Cocaine Use
Changes in behavior may be the next sign to appear. When someone starts acting strangely, or constantly sneaks around, it may be due to cocaine use.
The teenage years may present a dilemma, because during this time, people are changing anyways. Teenagers might act out or show aggression towards authority. Similarly, someone using cocaine may do a lot things that seem out of character like become violent, or recluse.
 Someone using cocaine might stay up later than usual, sleep at odd times during the day, spend a lot of time alone, and excessively use the bathroom without good reason. Suspicious activities may also include anonymous phone calls, and when you answer. when the person hangs up.
Someone using cocaine might stay up later than usual, sleep at odd times during the day, spend a lot of time alone, and excessively use the bathroom without good reason. Suspicious activities may also include anonymous phone calls, and when you answer. when the person hangs up.
Using large amounts of cocaine may increase a person’s euphoria, but at the same time it can lead to erratic, bizarre, and sometimes violent behavior. Cocaine use can lead to paranoia, anxiety, irritability, restlessness, and panic. Your loved one may seem energetic, talkative, euphoric, mentally alert, and be sensitive to sight, sound, and touch (NIDA).
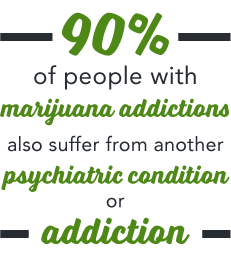
Some may even develop an obsessive compulsive disorder (OCD) as a result of their cocaine use—this occurrence of both mental and substance use disorder is referred to as a co-occurring disorder. With consistent results from epidemiological studies by the National Library of Medicine, subjects actively using cocaine (and also marijuana) were found to be at an increased risk for OCD.
4. Social Changes From Cocaine Use
Your loved one may stop spending time with lifelong friends as a result of their cocaine use. A teenager might even stop enrolling in extracurricular activities like sports, or academic clubs, and replace those social circles with other people who use drugs. An adult may avoid social situations with the exception of night clubs, bars, and other scenes where drug use is more widely accepted.
The people who aren’t using cocaine may not like their friend’s new found activity, and as a result stop hanging around them. The choice to cut ties with someone because of cocaine use can work from both sides. Sometimes it’s the person using cocaine who stop responding to their friends or family; maybe from fear of being rejected, or judged.
5. Physical Changes From Cocaine Use
 Sometimes the physical changes from cocaine use are the last thing people notice before they realize it’s a problem. Using cocaine temporarily decreases a person’s need for food and sleep. So as a result, they may lose a lot of weight, or even seem gaunt, or malnourished. Cocaine use may also come with the appearance of dark circles around the eyes.
Sometimes the physical changes from cocaine use are the last thing people notice before they realize it’s a problem. Using cocaine temporarily decreases a person’s need for food and sleep. So as a result, they may lose a lot of weight, or even seem gaunt, or malnourished. Cocaine use may also come with the appearance of dark circles around the eyes.
Cocaine can also result in a lot of adverse health consequences. Some of these aren’t as easy to determine as others, but may include:
- Constricted blood vessels
- Dilated pupils
- Cardiovascular complications
- Increased body temperature
- Heart rate
- Blood pressure
- Heart arrhythmia
- Heart attack
- Frequent headaches
- Seizures
- Gastrointestinal complications
- Nausea
- Stomach pain
- Respiratory complications
- Slowed breathing
- Coma
- Death
So repeated cocaine use not only puts a person at risk of becoming addicted or dependent upon the drug, it can also lead serious physical and mental health complications, and emergencies. In 2011, “cocaine was involved in 505,224 of the nearly 1.3 million visits to emergency departments for drug misuse or abuse,” (NIDA). If you believe someone you love is using cocaine, don’t give up on them, get help today.
Find Help For Cocaine Addiction And Dependence
It’s helps to remember that cocaine addiction is considered an disease, and even after a person changes from it, they’re still the same person. They just might need more help now. Contact DrugRehab.net today to speak to someone who understands addiction, and can tell you more about how to find cocaine addiction treatment for you or your loved one.
For More Information Related to “5 Signs Your Loved One Is Using Cocaine” Be Sure To Check Out These Additional Resources From DrugRehab.org:
- How Long Does Cocaine Stay In Your System?
- What is the Difference Between Cocaine and Crack?
- What Is “Freebase” Cocaine?
- Difference Between Amphetamines And Cocaine
- Signs of Speedball (Heroin with Cocaine) Use
Sources
National Institute on Drug Abuse – What Are The Short Term Effects of Cocaine Use?
National Institute on Drug Abuse – What is the Scope of Cocaine Use in the United States?
U.S. National Library of Medicine – Cocaine
U.S. National Library of Medicine – Cocaine Use and Other Suspected Risk Factors for Obsessive Compulsive Disorder






 Alcohol is a small molecule that interacts with a lot of different neurotransmitters in the brain, including: GABA, endorphins, dopamine, norepinephrine, glutamate, and adrenaline. Alcohol causes dependency, partly because as a person drinks, the dopamine in the reward pathway of the brain is increased.
Alcohol is a small molecule that interacts with a lot of different neurotransmitters in the brain, including: GABA, endorphins, dopamine, norepinephrine, glutamate, and adrenaline. Alcohol causes dependency, partly because as a person drinks, the dopamine in the reward pathway of the brain is increased. There are three stages to alcohol withdrawal, the first of which can begin as early 6 hours after a person’s peak intoxication. The stages go from mild to moderate to severe, and can last anywhere from 5 to 7 days. Generally after a week, the majority of withdrawal symptoms will have subsided, however, some may persist for several weeks without proper treatment.
There are three stages to alcohol withdrawal, the first of which can begin as early 6 hours after a person’s peak intoxication. The stages go from mild to moderate to severe, and can last anywhere from 5 to 7 days. Generally after a week, the majority of withdrawal symptoms will have subsided, however, some may persist for several weeks without proper treatment.




 This is only a potential scenario, and doesn’t apply to everyone—the point is that though not everyone abuses prescription drugs for the same reason, all of our minds are wired the same way to crave things that make us feel good.
This is only a potential scenario, and doesn’t apply to everyone—the point is that though not everyone abuses prescription drugs for the same reason, all of our minds are wired the same way to crave things that make us feel good.

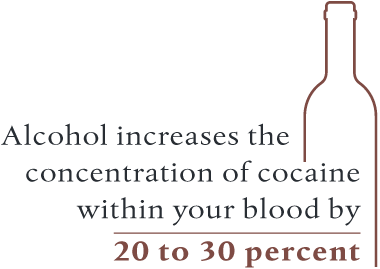 For individuals who aren’t accustomed to consuming alcohol with crack, the potential for a fatal overdose skyrockets. Alcohol can actually make it easier for your body to absorb cocaine, which increases the concentration of cocaine within your blood by 20 to 30 percent. From this effect, a person could overdose if they take an amount they are typically used to when using the drug alone.
For individuals who aren’t accustomed to consuming alcohol with crack, the potential for a fatal overdose skyrockets. Alcohol can actually make it easier for your body to absorb cocaine, which increases the concentration of cocaine within your blood by 20 to 30 percent. From this effect, a person could overdose if they take an amount they are typically used to when using the drug alone.




 Codeine has been mixed with different drugs to treat various medical conditions, most commonly acetaminophen. There are various strengths of this drug combination, indicated in the title of the drug as Tylenol 2, Tylenol 3, and Tylenol 4. Tylenol 4 is the most potent of these medications, containing 60mg of codeine and 325mg of acetaminophen.
Codeine has been mixed with different drugs to treat various medical conditions, most commonly acetaminophen. There are various strengths of this drug combination, indicated in the title of the drug as Tylenol 2, Tylenol 3, and Tylenol 4. Tylenol 4 is the most potent of these medications, containing 60mg of codeine and 325mg of acetaminophen. While reducing the amount and frequency of opioids if you have a substance abuse issue is important, quitting abruptly can be extremely dangerous. Because your brain has become accustomed to a certain level of opioids binding with your opioid receptors, your body considers this new chemical balance to be the norm. If you suddenly stop taking opioids, then this level will come down too rapidly, resulting in withdrawal symptoms.
While reducing the amount and frequency of opioids if you have a substance abuse issue is important, quitting abruptly can be extremely dangerous. Because your brain has become accustomed to a certain level of opioids binding with your opioid receptors, your body considers this new chemical balance to be the norm. If you suddenly stop taking opioids, then this level will come down too rapidly, resulting in withdrawal symptoms.
 Suboxone is a fairly new drug to the addiction treatment market. Intended to treat all types of opioid addiction in adults, Suboxone is actually a combination of two different types of drugs; buprenorphine and naloxone. Often prescribed for pain control,
Suboxone is a fairly new drug to the addiction treatment market. Intended to treat all types of opioid addiction in adults, Suboxone is actually a combination of two different types of drugs; buprenorphine and naloxone. Often prescribed for pain control, 
 With this tolerance generally comes increased or more frequent consumption of the drug, which can lead to serious long-term effects down the road. These
With this tolerance generally comes increased or more frequent consumption of the drug, which can lead to serious long-term effects down the road. These 
 Alcohol withdrawals
Alcohol withdrawals
 In summary, alcohol withdrawal is not only a result of a physical demand of the chemical, but also the cognitive function in trying to maintain normal function.
In summary, alcohol withdrawal is not only a result of a physical demand of the chemical, but also the cognitive function in trying to maintain normal function.







 The
The