Imodium, which contains the active ingredient loperamide, is an over-the-counter medication used to treat diarrhea. It had long been thought that this medication did not hold serious potential for abuse. In fact, in 1980, a study was conducted to study just this. The study compared the effects of loperamide to that of codeine, an addictive opiate; and determined “loperamide poses little threat of potential abuse,” the study also noted that participants who used higher amounts of the medication (12-60mg) reported that it “was “liked” little or not at all, and was identified as “dope” at a frequency less than that for a threshold dose of oral codeine.”
Now, nearly forty years later, it’s becoming clear that these determinations can in certain circumstances prove false. What medical experts are finding—as is supported by the surge of personal accounts that are cropping up on the internet—is that this is not the case. Loperamide is becoming increasingly abused by individuals that are using it to either self-treat opiate dependence or withdrawal, or to seek the euphoria associated with these drugs. It is being increasingly misused in proportions that, in the most extreme reported usage, exceed the recommended dosage by amounts as high as 25 to nearly 50 times.
Why Are People Misusing This Drug?
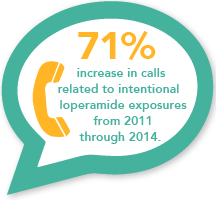
A recent study published in the Annals of Emergency Medicine found that misuse and abuse of Imodium is on the rise. The study’s authors wrote “our data are consistent with national poison center data, which demonstrated a 71% increase in calls related to intentional loperamide exposures from 2011 through 2014.” They cited the following reasons why this abuse is becoming so prevalent: “loperamide’s accessibility, low cost, over-the-counter legal status, and lack of social stigma associated with its use contribute to its potential for abuse.”
 For those that are struggling with an opiate addiction and are either not able to find or afford their drug of choice or are struggling with the symptoms of withdrawal as they attempt to stop using it, taking loperamide seems like a simple way to obtain their goals.
For those that are struggling with an opiate addiction and are either not able to find or afford their drug of choice or are struggling with the symptoms of withdrawal as they attempt to stop using it, taking loperamide seems like a simple way to obtain their goals.
Some people may unknowingly stumble into this misuse as they take the drug to treat constipation which is one of the most common side effects of an opiate withdrawal. In the process of taking the drug for this purpose, they may begin adjusting the dosage on their own accord as they find that the drug is moderating other withdrawal symptoms as well. Other people begin taking excess amounts of the drug right off the bat in the hopes that it will substitute the other opiate(s) they were taking and alleviate their concerns.
 Though the effect is minimal, and not encountered by every person that takes this drug in large proportions, some people take massive doses for recreational purposes and claim that they experience a more minimal sense of the high or euphoria that other opiates create.
Though the effect is minimal, and not encountered by every person that takes this drug in large proportions, some people take massive doses for recreational purposes and claim that they experience a more minimal sense of the high or euphoria that other opiates create.
Currently, there are no restrictions on the amount of this drug that an individual can buy. For this reason people are able to take this medication in large proportions in an attempt to mimic the effect of other opiate drugs.
How Does Imodium Cause These Effects?
Opiates bind to one or both of two locations where opioid receptors are located within the human body—within the brain or within the gut. Typically, opiates that are commonly abused, including illicit drugs such as heroin or prescription painkillers, bind to the receptor sites within the brain. It is the interaction of the drug on these binding sites that causes the euphoric feelings that individuals that abuse opiates seek.
A second study, also focusing on the dangers of loperamide abuse, published in the journal Clinical Toxicology describes loperamide as having “peripheral mu-opioid receptor activity.” As a result, if used as recommended, it has a limited ability to pass through the blood-brain barrier preventing it from binding to the receptors within the brain in any significant capacity. Instead, it binds primarily to the ones within the gut, specifically those within the intestines.
When used properly within this therapeutic range only miniscule amounts of the drug pass through the blood-brain barrier. The danger and damage occurs when a person consumes an amount in excess of the recommended dosage. In these quantities the drastically heightened levels of loperamide in the system allow for larger amounts of the drug to pass through the blood-brain barrier causing a feeling, that though significantly less, is claimed by some to mimic the effect of other more serious opiates or temper the uncomfortable feelings of withdrawal.
Over-The-Counter Does Not Mean Safe
Within groups that misuse this and other OTC medications there is a common misconception that because something is sold without a prescription that it is automatically safe. This is true if the medication is used within the bounds of its intended purposes, meaning that the purpose, dosage, and frequency of use all fall within the perimeters of what the medication is manufactured for. When a medication is used beyond this, in proportions that are greater than the intended dosage, risk and danger rise proportionately.
What Are The Dangers Of Imodium Abuse?
The study presented by the Annals of Emergency Medicine found that this use is accompanied by dangerous and even deadly results. It detailed that “in the overdose setting it causes significant central nervous system and respiratory depression, cardiac dysrhythmias, and death.” In addition to these risks, the U.S. National Library of Medicine’s DailyMed reported that an overdosage can cause “urinary retention, paralytic ileus and CNS depression.”
 The study’s authors spoke of two individuals that took massive quantities of loperamide and subsequently overdosed. Emergency services were contacted and what followed for both failed to prove life-saving. Despite medical intervention and support, including “manual cardiopulmonary resuscitation (CPR), naloxone, and standard advanced cardiac life support (ACLS),” both individuals died prior to arriving at the emergency room.
The study’s authors spoke of two individuals that took massive quantities of loperamide and subsequently overdosed. Emergency services were contacted and what followed for both failed to prove life-saving. Despite medical intervention and support, including “manual cardiopulmonary resuscitation (CPR), naloxone, and standard advanced cardiac life support (ACLS),” both individuals died prior to arriving at the emergency room.
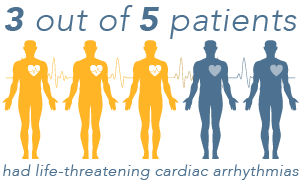
The Clinical Toxicology study detailed five cases of loperamide abuse, it reported that “3 of the 5 patients had life-threatening cardiac arrhythmias. One of the patients experienced a second life-threatening arrhythmia after he resumed loperamide abuse.” The good news is, that this study reported that “discontinuation of loperamide resulted in complete resolution of cardiac conduction disturbances.”
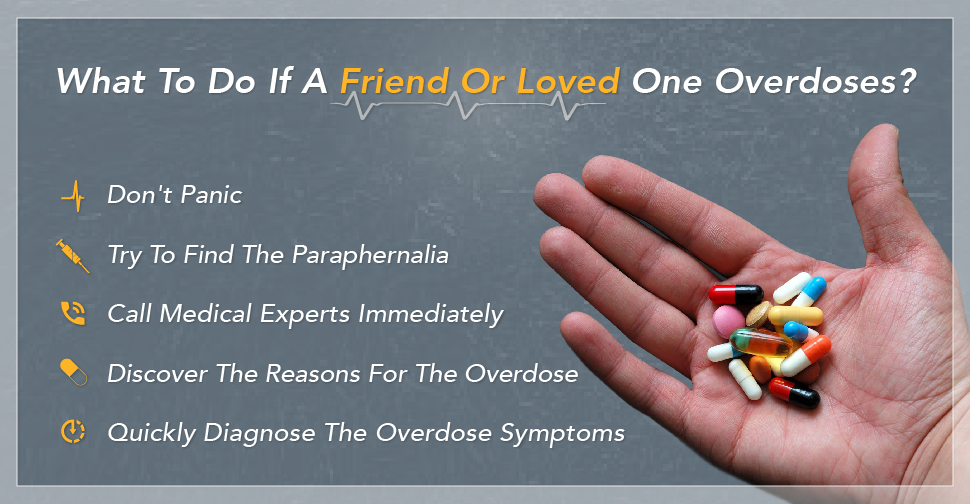
As with any drug use, risk may rise if this medication is combined with other drugs, especially drugs that suppress the CNS. If you, or someone you love, has any fear that you’ve overdosed on loperamide seek medical attention immediately.
Don’t Manage Your Addiction Or Withdrawal On Your Own
 Attempting to undergo the withdrawal process on your own can be daunting and at times dangerous. It is never recommended that anyone, under any circumstances, self-medicate the symptoms of withdrawal. This process should be supervised by trained professionals that can direct and provide you with the care and medical and emotional support that is necessary within this process.
Attempting to undergo the withdrawal process on your own can be daunting and at times dangerous. It is never recommended that anyone, under any circumstances, self-medicate the symptoms of withdrawal. This process should be supervised by trained professionals that can direct and provide you with the care and medical and emotional support that is necessary within this process.
If you’re misusing or abusing Imodium or any other product that contains loperamide, struggling with an opiate addiction, wanting to quit using but are fearful of facing withdrawal symptoms, or find that you’re self-medicating your withdrawal symptoms in any other way, please allow us to offer you the help and assistance that can be crucial to obtaining sobriety and finding lasting recovery. Here, at Drugrehab.org, we have a patient, trained, and compassionate staff that is standing by to help you make the best decision about your care today.





 For Treatment Of Opiate Addiction: For those that suffer from opiate dependence, this drug is used as a part of medication-assisted treatment (MAT) or therapy to help people taper off opiates. Buprenorphine binds to and occupies the same opioid receptors as the abused drug, creating the same effects. It is for this reason that cravings are reduced. Like any opiate, buprenorphine works on the Central Nervous System, but in this case it causes decreased withdrawal symptoms.
For Treatment Of Opiate Addiction: For those that suffer from opiate dependence, this drug is used as a part of medication-assisted treatment (MAT) or therapy to help people taper off opiates. Buprenorphine binds to and occupies the same opioid receptors as the abused drug, creating the same effects. It is for this reason that cravings are reduced. Like any opiate, buprenorphine works on the Central Nervous System, but in this case it causes decreased withdrawal symptoms.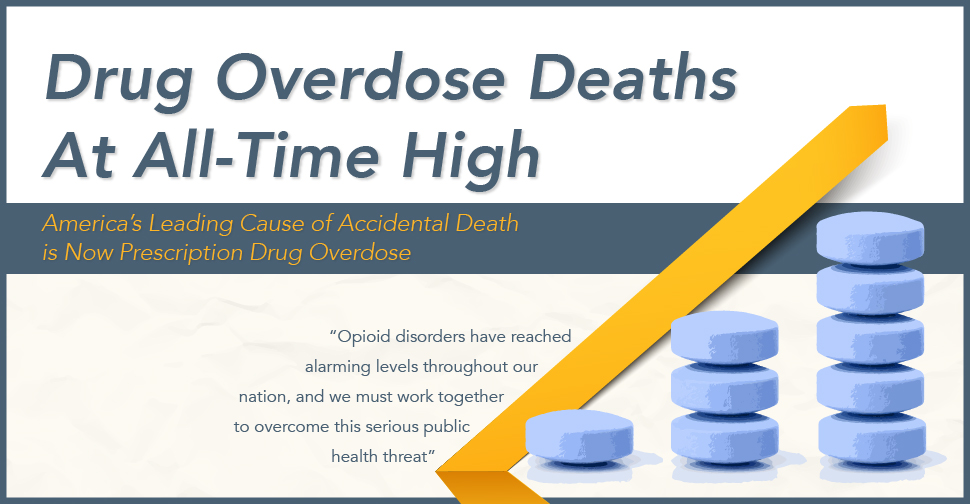

 Grieving Families Break Taboos, Humanize Drug Addiction Crisis
Grieving Families Break Taboos, Humanize Drug Addiction Crisis The Murray and Avitabile families fought the ravages of addiction in Massachusetts, where the epidemic is especially dire. The state health department reports 1,089 overdose deaths in Massachusetts in 2014 – up 20 percent over the previous year. At a recent community forum in Wilmington, officials revealed that the Merrimack Valley region leads the nation in heroin sales and usage, The Lowell Sun newspaper reported.
The Murray and Avitabile families fought the ravages of addiction in Massachusetts, where the epidemic is especially dire. The state health department reports 1,089 overdose deaths in Massachusetts in 2014 – up 20 percent over the previous year. At a recent community forum in Wilmington, officials revealed that the Merrimack Valley region leads the nation in heroin sales and usage, The Lowell Sun newspaper reported.