
Massachusetts governor Deval Patrick declared a state of emergency in March of 2014, requesting additional resources to combat a wave of opiate overdoses in his state. The number of overdose deaths in Massachusetts increased a staggering 90 percent in the past decade, an increase that parallels a rise in the number of opiate medications being prescribed by doctors.
Highly addictive prescription opiate medications like OxyContin were being peddled to unsuspecting Americans by doctors who were told the drug was not addictive by big pharmaceuticals. As doctors became suspect of the drug, and government regulations restricted its availability, the price of prescription opiates rose. Those now addicted to the prescription medications were all too willing to switch over to the far less expensive, but more dangerous street alternative, heroin.
Mechanism For Opiate Addiction
The mechanisms for opiate addiction relate to a number of social, economic, and genetic factors. As with any addiction, opiates stimulate a part of the brain associated with pleasure and reward, but the addiction begins with that first use. What compels that first use, in the case of this dramatic spike in heroin use, can be as innocent as a complaint to your doctor about pain.
When a person begins taking a prescription opiate pain reliever, the drug binds and activates opioid receptors located in the brain and along the central nervous system. It is a synthetic equivalent to the body’s own pain-response system, but lowers the pain threshold far more than possible naturally. This reduction in pain sends a signal to a region of the brain known as the nucleus accumbens. This part of the brain, also known as the brain’s pleasure center, is an ingenious motivator developed through millions of years of evolution.
Here’s how it works: When prehistoric man found a good source of food high in protein and fat, his brain took notice. The man’s body is flooded with dopamine, making him feel satiated and content. This reward is the body’s way of encouraging the man to seek out this food source again. At the same time, as this process is unfolding, the man’s brain is mapping his surroundings, noting patterns in the environment that will make locating this food source in the future more efficient.
It’s an ingenious system that worked for humans for hundreds of thousands of years, but with the advent of opiates, this same protective mechanism turns our bodies and minds against us. Opiates initiate a powerful dopamine response, which our bodies perceive as important to our survival. The response is many times stronger than that associated with basic needs like food and water, and the brain quickly begins associating opiates with survival.
Moreover, opiates affect the release of endorphins, dopamine, and even GABA, altering the natural effects of these neurotransmitters normally associated with the body’s natural ability to reduce pain. The more someone uses opiate medications, the less the body relies on its own process, leading to a physical dependency on the drug. The person no longer uses the drug to achieve a high, but must use the drug to keep withdrawal symptoms at bay.
Prescription Opiates And The Affordable And Deadly Alternative
The rise of prescription opiate pain medications like OxyContin caused many to develop a dependence on the medication. As the price of the medication increased, or doctors became weary of prescribing the drugs, people had to look elsewhere to satiate their addiction. Heroin was a cheap alternative and its availability made it an easy alternative.
In a recent episode of Anthony Bourdain’s Parts Unknown, the chef and former heroin addict talked openly about the epidemic sweeping states like Massachusetts. Traveling from restaurant to restaurant, he interwove his usual foodie escapades with stories from middle and upper class Americans on how the epidemic of heroin has stolen lives and changed small towns in ways never imagined.
In the shadow of skyrocketing heroin-related overdoses in a state with high socioeconomic wealth, Bourdain asserted this recent spread of heroin into middle and upper-class America shows there really is no protective bubble to save any one race or type of person from addiction.
“Maybe now, now that it’s really come home to roost, now that it’s the high school quarterback, your next-door neighbor, your son, your daughter, now that grandma is as likely to be a junkie as anybody else, we’ll accept that there has never been a real war on drugs. ‘War on drugs’ implies an us versus them, and all over this part of America, people are learning there is no them. There is only us. And we’re going to have to figure this out together.”
The Doctor Patient Opiate Dilemma
Unfortunately, another factor that fueled the dramatic spike in opiate addiction was a failure by medical professionals in diagnosing the problem. Stereotypes that people who use drugs are socio-economically disadvantaged or people of color persist in this country. Despite the fact that race has nothing to do with addiction risk factors, a physician is far less likely to talk with an upper-class white woman about opiate addiction than a person of color or someone in poverty. So, when heroin began invading the homes of middle and upper-class America, the stereotype masked the problem until it ravaged entire communities.
The national response to combat the high rates of overdose deaths is funding training programs for first responders, police, and the public in the use of opioid antagonist medications. However, far more public awareness is needed as well as cooperation with medical professionals to assess and address addiction risk factors before and after prescribing opiate pain medications.
Narcan Response To Opiate Overdose
Opioid antagonists medications like narcan bind with opioid receptors without activating the receptor, so someone overdosing on heroin who receives the drug will see a reversal of the central nervous system depressing effects.
The drug has been in use since the 1960s, but in light of recent surges in overdose deaths, public initiatives educating people on how to access and use narcan have begun. Police, who never used to carry narcan, are now first in line to respond to an overdose. This means faster administration and a success rate higher than 90% in reducing the number of deaths associated with heroin overdose, when administered properly.
Get Help Today For Your Opiate Addiction
 An addiction to opiates is one of the most challenging to overcome, but recovery is possible and manageable through a comprehensive treatment programs and ongoing support. If you are currently battling an addiction to opiate pain medications or heroin, DrugRehab.org can offer a lifeline, connecting you with professional support and treatment options available to meet your individual needs. Don’t become a statistic, contact us and speak with someone in confidence today and discover a better life in recovery.
An addiction to opiates is one of the most challenging to overcome, but recovery is possible and manageable through a comprehensive treatment programs and ongoing support. If you are currently battling an addiction to opiate pain medications or heroin, DrugRehab.org can offer a lifeline, connecting you with professional support and treatment options available to meet your individual needs. Don’t become a statistic, contact us and speak with someone in confidence today and discover a better life in recovery.
For More Information, Be Sure To Check Out These Additional Resources From DrugRehab.org:
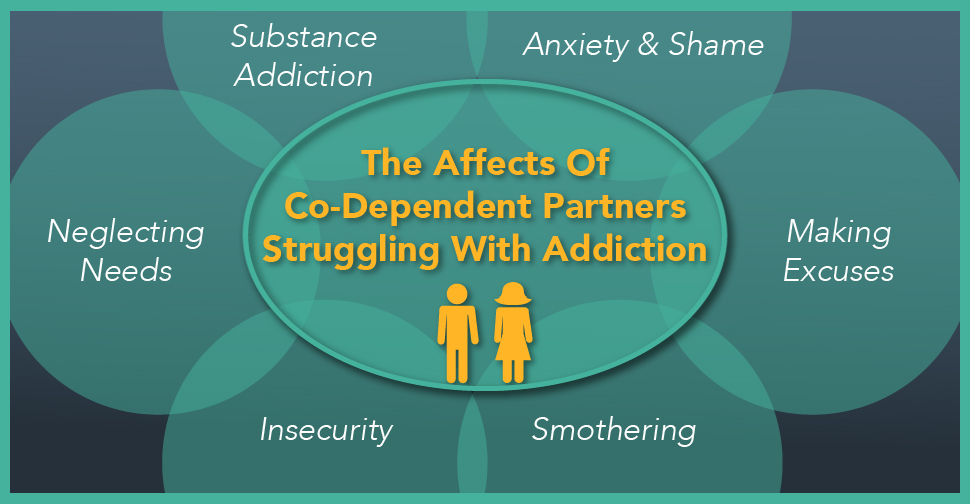
 If you find yourself in a co-dependent relationship with an addict or are struggling with addiction yourself, contact us today. We can help you find treatment for both issues. Addiction is a complex thing, and rarely affects just one person in a situation. Let us assist you in discovering how to best care for everyone touched by addiction in your life.
If you find yourself in a co-dependent relationship with an addict or are struggling with addiction yourself, contact us today. We can help you find treatment for both issues. Addiction is a complex thing, and rarely affects just one person in a situation. Let us assist you in discovering how to best care for everyone touched by addiction in your life.




 Drugs come in and out of fashion as easily as the clothes on our backs, a depressing, but true notion. Unfortunately, effectiveness measured against addiction risk isn’t the key determinant for whether someone is prescribed a powerful opiate for pain or a benzodiazepine medication for anxiety or insomnia. Instead, outdated and often misinformed literature, powerful ad campaigns by pharmaceutical companies, and drug representatives pushing for use of their company’s product, guide both the public’s perception of the effectiveness and uses of these drugs, as well as the physicians prescribing medications to their patients.
Drugs come in and out of fashion as easily as the clothes on our backs, a depressing, but true notion. Unfortunately, effectiveness measured against addiction risk isn’t the key determinant for whether someone is prescribed a powerful opiate for pain or a benzodiazepine medication for anxiety or insomnia. Instead, outdated and often misinformed literature, powerful ad campaigns by pharmaceutical companies, and drug representatives pushing for use of their company’s product, guide both the public’s perception of the effectiveness and uses of these drugs, as well as the physicians prescribing medications to their patients.
