Far too often, family members of addicted individuals become enablers, that is their actions actually make it easier for a substance-abusing lifestyle to continue. Examples include being in denial, making excuses for a person or covering up for them, taking on extra responsibilities, certain types of financial assistance, and using or providing the substance.
Watching A Family Member Go Through Addiction Can Upend Your Life
When addiction overtook your family member’s life, your world suddenly turned upside down. You may be experiencing an array of confusing and intense emotions, ranging from betrayal, blame, shame, resentment, fear, anger, and sadness. But despite this, you still love them deeply and find that you want to help them.
Within all of this, you might question your role, both before and during the addiction. These emotions and thoughts are understandable and experienced by many within these situations. It’s how you handle them which makes the difference, both within your life and your family member’s.
5 Ways People Enable Their Addicted Loved One
It’s our nature to love and seek love. We do this by words and actions of affirmation and by offering support when someone is in need. But when a person is addicted to drugs or alcohol, the line between helpful and healthy and damaging and enabling becomes easily blurred. So what is enabling?

When you enable a drug abuser you’re preventing them from experiencing the full effect of their addiction and making it easier to keep using. By doing so, it becomes difficult for them to see why they need to change and also prevents them from developing the acceptance and motivation to do so.
Below are five ways people end up enabling a loved one.
1. Feeding Denial
While denial can be a natural part of accepting a person’s substance abuse, when it continues past a reasonable point, it can become profoundly enabling. Looking the other way only serves to harm both them and you.
Examples include:
- Blaming it on yourself. Convincing yourself that something you did drove them to drink or use in the first place and continues to do so. This can be part of a larger problem, but it’s often intertwined with denial.
- Ignoring family and friends when they implore you to recognize the addiction.
- Ignoring signs of addictive behavior and the damage it’s doing to a person’s life (finding hidden bottles and leaving them there or throwing them out without saying a word).
- Lying to yourself (when a person’s sick or volatile from the substance, saying it’s the flu or a bad day).
- Believing them when they say they can beat it on their own. Addicted people have the highest chance of success with comprehensive treatment.
- Suppressing your emotions. Not allowing yourself to feel the toll of the addiction is a form of denial.
Being aware and proactive about your loved one’s addiction can help you to help them get treatment faster and make it more obvious to them that they need help.
2. Making Excuses And/Or Covering Up For A Person
This often stems from denial, codependency, or even just exhaustion and frustration.
Examples include:
- Calling in sick to work for them if they’re drunk, high, hungover, or sick from using.
- Covering up for them so they don’t get in trouble at school or with the law.
- Covering up their actions to avoid a fight or other loved ones finding out/getting angry at them.
- Making excuses for their substance abuse (they’re stressed out, school or their job is tough, etc.).

It can wear you out to watch a loved one fall into the depths of addiction, and sometimes it just feels easier to do things yourself. But know that in the long run these, and other actions like them, are only serving to perpetuate the vicious cycle that is the addictive lifestyle.
3. Picking Up The Slack
When a person is addicted, responsibilities at home or at work often become ignored. This can place a lot of extra stress on you, both mentally, emotionally, and even financially.
Examples include:
- Doing extra chores around or outside of the house.
- Taking over their responsibilities with children or elderly parents.
- Working extra hours so they can cut back on their job responsibilities (or even quit).
While it’s important that you support them, don’t do things for them that they should do on their own. Doing so not only gives them more time to use, but this form of enabling takes away a major incentive for change as a person’s insulated from seeing and feeling the adverse effects of their drug-seeking and using.
4. Financially
We don’t ever want our loved ones to suffer, and when you see your family member losing the battle to addiction, it can be easy to lend a helping hand without realizing the full impact.
Examples include
- Giving them money for food, bills, or utilities. They can use this money for drugs. Or, even if they use it for these things, it still gives them more resources to purchase drugs.
If you want to help out financially, consider pitching in for treatment costs, should you be able to afford it.
5. Using With Them Or Providing The Substance
Now this may be alcohol, a legal and highly social drug; marijuana, which is legal in limited places; or an illicit drug. Just because a drug is legal or socially acceptable doesn’t mean it’s not harmful or that it’s okay to do with an addicted person.
Examples include:
- Using the substance with them even when you know they have a problem, because you want to have a “fun time” with them.
- Buying the substance for them (beer, wine, marijuana, etc.) because you figure they’ll do it anyways and at least you know what/how much they’re using.

Keep in mind, using around a person can be bad too. Some people in recovery can tolerate this, but many cannot. For these people, seeing and smelling a substance can be an intense trigger for relapse. And any time you’re using a drug (even alcohol) you’re exposing yourself to risks too.
If you recognize any of these enabling patterns in yourself it’s time to take a step back and reevaluate how you interact with your family member.
Ways To Overcome Enabling And Give Them The Help They Need
If you’re caught up in unhealthy patterns of enabling, or if you’re concerned you might fall into them, here’s some ways you can offer healthy support. Being mindful of your thoughts, emotions and behaviors, and the ways by which they affect you and your loved one, can help to protect you both.
Be Patient, But Not Lenient: Addiction makes it difficult to think clearly and prioritize healthy behaviors. Try and understand this as you encounter your loved one, but don’t let them take advantage of your understanding, or use it as an excuse.
Be Proactive Instead Of Reactive: When faced with a situation where you could resort to enabling, stop and think. Rather than reacting in an emotional way, take time to think about your actions. Ask yourself: “If I do this, am I really helping them? Or am I making it easier for them to continue using?” In these moments, think of ways you could support them so that they find inner strength or have access to tools to take control over these situations themselves.
Be Real With Them: It’s easy to think we need to sanitize our emotions and reactions in tough situations. But if they see the adverse effects of their addiction on you, it might help them to recognize that they have a problem and that they need help.
Do Healthy Things Together: During treatment this may mean taking part in a counseling session or recreational activity. And after, it could be as simple as taking a walk after dinner, going to a movie, or working on a do-it-yourself project together.
Don’t Offer A Solution, Build One: Instead of creating the solution, help your loved one learn how to take more positive steps to find one on their own. For instance, instead of giving them money when they ask, sit down with them and help them prepare a resume, look for a job, and/or create a budget.
Get Support: Consider joining a support group. If you take steps to help yourself, you’re providing inspiration and a proactive example for change to your loved one. This might help them become more ambitious to do the same. Counseling can be immensely beneficial as well.

Practice Tough Love: In these situations, while saying “no” can be the hardest thing, it’s the best thing. Forced to deal with the repercussions of their addiction, a person will be more apt to take strides to seek help and start changing.
Research Treatment Options: The best way to support your loved one in living a drug-free life is to help them get the treatment they need. With our help, you can research their drug of abuse, find the best treatment options, and even examine ways to cover the cost of treatment.
Take Charge And Stop The Cycle Of Enabling Today
Fortunately, it’s never too late to help, or to learn more healthy ways to look out for your loved one. If your family member is addicted, they need your love and support now more than ever. Let DrugRehab.org help you with these things. Contact us today.
For More Information Related to “5 Ways People Enable Their Addicted Loved One” Be Sure To Check Out These Additional Resources From DrugRehab.org:




 One of the first signs of cocaine use will appear when an individual runs out of money. Cocaine is one of the more expensive drugs, and the high from it doesn’t last very long so one binge can be costly. According to the
One of the first signs of cocaine use will appear when an individual runs out of money. Cocaine is one of the more expensive drugs, and the high from it doesn’t last very long so one binge can be costly. According to the  Someone using cocaine might stay up later than usual, sleep at odd times during the day, spend a lot of time alone, and excessively use the bathroom without good reason. Suspicious activities may also include anonymous phone calls, and when
Someone using cocaine might stay up later than usual, sleep at odd times during the day, spend a lot of time alone, and excessively use the bathroom without good reason. Suspicious activities may also include anonymous phone calls, and when  Sometimes the physical changes from cocaine use are the last thing people notice before they realize it’s a problem. Using cocaine temporarily decreases a person’s need for food and sleep. So as a result, they may lose a lot of weight, or even seem gaunt, or malnourished. Cocaine use may also come with the appearance of dark circles around the eyes.
Sometimes the physical changes from cocaine use are the last thing people notice before they realize it’s a problem. Using cocaine temporarily decreases a person’s need for food and sleep. So as a result, they may lose a lot of weight, or even seem gaunt, or malnourished. Cocaine use may also come with the appearance of dark circles around the eyes. 

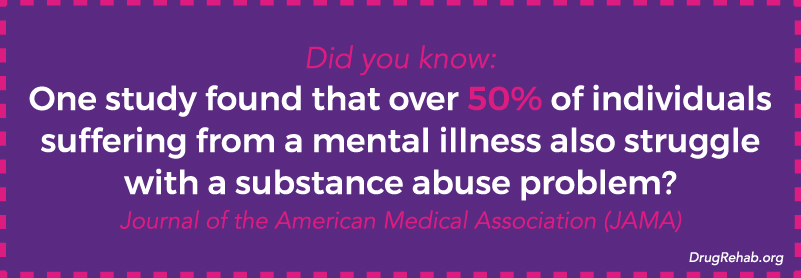
 Mental Illness
Mental Illness




 Alcohol is a small molecule that interacts with a lot of different neurotransmitters in the brain, including: GABA, endorphins, dopamine, norepinephrine, glutamate, and adrenaline. Alcohol causes dependency, partly because as a person drinks, the dopamine in the reward pathway of the brain is increased.
Alcohol is a small molecule that interacts with a lot of different neurotransmitters in the brain, including: GABA, endorphins, dopamine, norepinephrine, glutamate, and adrenaline. Alcohol causes dependency, partly because as a person drinks, the dopamine in the reward pathway of the brain is increased. There are three stages to alcohol withdrawal, the first of which can begin as early 6 hours after a person’s peak intoxication. The stages go from mild to moderate to severe, and can last anywhere from 5 to 7 days. Generally after a week, the majority of withdrawal symptoms will have subsided, however, some may persist for several weeks without proper treatment.
There are three stages to alcohol withdrawal, the first of which can begin as early 6 hours after a person’s peak intoxication. The stages go from mild to moderate to severe, and can last anywhere from 5 to 7 days. Generally after a week, the majority of withdrawal symptoms will have subsided, however, some may persist for several weeks without proper treatment.

 A speedball refers to a mixture of depressants and stimulants; it’s a form of polysubstance abuse. A few examples of a speedballing are alprazolam with methamphetamine, alcohol with amphetamines, or the most common speedball, heroin with cocaine.
A speedball refers to a mixture of depressants and stimulants; it’s a form of polysubstance abuse. A few examples of a speedballing are alprazolam with methamphetamine, alcohol with amphetamines, or the most common speedball, heroin with cocaine. Most of the time heroin and cocaine are diluted with non mood altering substances such as starch, sugar, flour, powdered milk, talcum powder, or even rat poisoning. So there isn’t always a way to tell what either drug has been cut with, thus the purity of each drug isn’t always clear. An amount that proved to be “safe” last time someone mixed heroin and cocaine, could be a fatal dose this time.
Most of the time heroin and cocaine are diluted with non mood altering substances such as starch, sugar, flour, powdered milk, talcum powder, or even rat poisoning. So there isn’t always a way to tell what either drug has been cut with, thus the purity of each drug isn’t always clear. An amount that proved to be “safe” last time someone mixed heroin and cocaine, could be a fatal dose this time.

 This is only a potential scenario, and doesn’t apply to everyone—the point is that though not everyone abuses prescription drugs for the same reason, all of our minds are wired the same way to crave things that make us feel good.
This is only a potential scenario, and doesn’t apply to everyone—the point is that though not everyone abuses prescription drugs for the same reason, all of our minds are wired the same way to crave things that make us feel good.


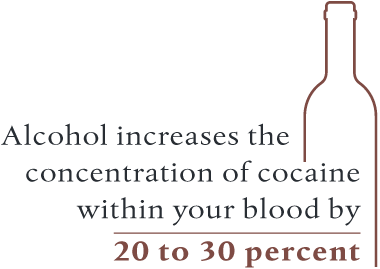 For individuals who aren’t accustomed to consuming alcohol with crack, the potential for a fatal overdose skyrockets. Alcohol can actually make it easier for your body to absorb cocaine, which increases the concentration of cocaine within your blood by 20 to 30 percent. From this effect, a person could overdose if they take an amount they are typically used to when using the drug alone.
For individuals who aren’t accustomed to consuming alcohol with crack, the potential for a fatal overdose skyrockets. Alcohol can actually make it easier for your body to absorb cocaine, which increases the concentration of cocaine within your blood by 20 to 30 percent. From this effect, a person could overdose if they take an amount they are typically used to when using the drug alone.
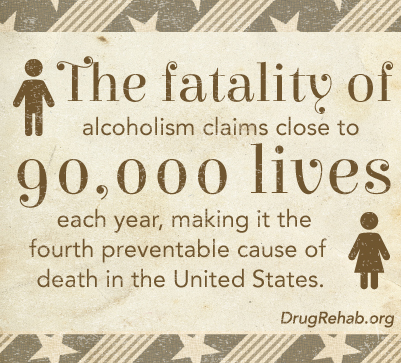 Alcohol abuse
Alcohol abuse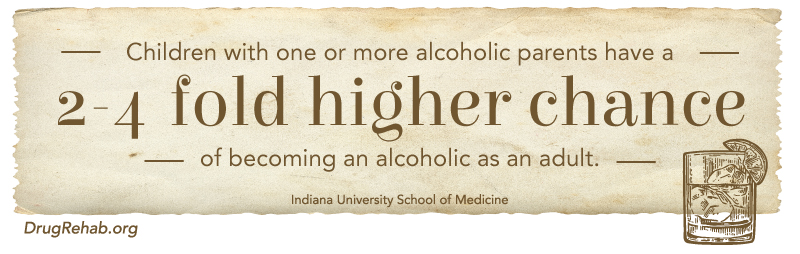






 On the opposite side of the ring, naloxone is actually an antagonist that blocks opioid receptors by sticking to them without activating them. Naloxone on its own is a common drug used by emergency medical respondents to reverse potentially lethally overdoses on drugs such as heroin.
On the opposite side of the ring, naloxone is actually an antagonist that blocks opioid receptors by sticking to them without activating them. Naloxone on its own is a common drug used by emergency medical respondents to reverse potentially lethally overdoses on drugs such as heroin.


 Women who have suffered with
Women who have suffered with 
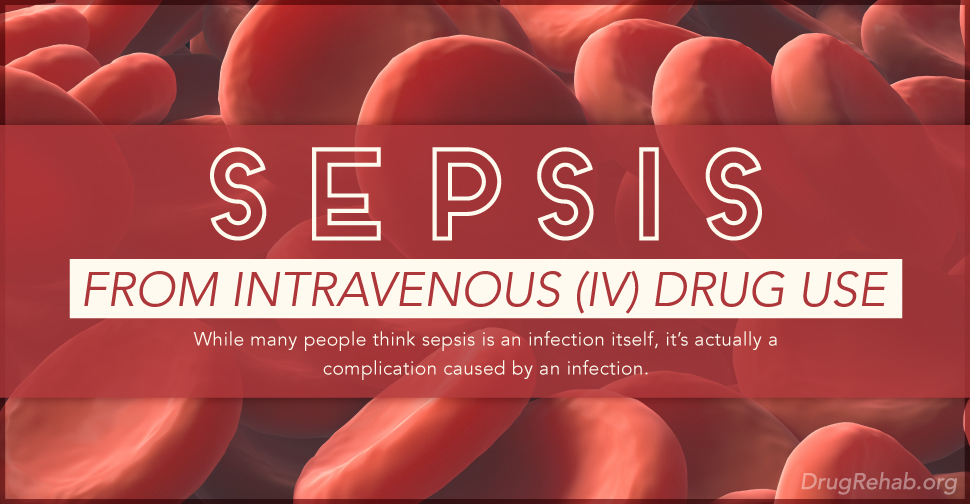


 Again, cotton balls are commonly used for this purpose since they are so cheap and readily available. Once a drug is in liquid form, a person draws the substance through the filter and into the syringe. The forearm is a
Again, cotton balls are commonly used for this purpose since they are so cheap and readily available. Once a drug is in liquid form, a person draws the substance through the filter and into the syringe. The forearm is a 
 Immunologic theory: Users have antibodies for the cotton which cause a reaction after injection
Immunologic theory: Users have antibodies for the cotton which cause a reaction after injection