Crohn’s disease causes your digestive tract to become severely inflamed. Its often incapacitating symptoms lead some individuals to self-medicate by substance abuse. Some even become addicted to their prescribed painkillers because of this. Whether it be alcohol or other drugs, these substance can lead to addiction and aggravate the disease.
Crohn’s disease currently has no cure. For an individual with Crohn’s, this prognosis can seem quite dim, especially when paired with the life-altering symptoms the disease produces. But with the proper lifestyle, therapies, and treatment, Crohn’s can be successfully managed, and so can an addiction.
What Is Crohn’s Disease?
Crohn’s disease is a type of inflammatory bowel disease (IBD). This inflammation causes distress to a person’s digestive tract, specifically the small intestine and colon. Sometimes the symptoms temporarily subside, this is called remission.
While symptoms can be mild, in its most extreme manifestations, “Crohn’s disease can be both painful and debilitating, and sometimes may lead to life-threatening complications,” according to Mayo Clinic.

This reality may lead some individuals to self-medicate their pain or emotional symptoms with drugs or alcohol. Doing so will only complicate matters further, and in many cases it will intensify the symptoms even more.
Is It Dangerous To Have Both?
Crohn’s can mask certain symptoms of substance abuse and vice versa. This can make it difficult to identify the root of the problem in some individuals and forestall treatment.
Depending on the drug of abuse, both diseases can create similar symptoms, such as abdominal cramping, diarrhea, weight loss, a suppressed appetite, malnourishment, and dehydration, among others. Individuals with Crohn’s may try to blame the side effects of their drug abuse on it in an attempt to hide their addiction.
These effects (especially malnourishment and dehydration) can become dangerous when compounded by chronic drug use and Crohn’s. Both diseases have also been linked to increased rates of anxiety, depression, and suicide.
The Emotional Strain Of Crohn’s Can Lead To Substance Abuse
It can be difficult to cope with a serious disease like Crohn’s and the many ways it alters your life. Over time, a person’s mental and emotional health can become seriously compromised, in a way which fosters substance abuse.
 Mental Illness
Mental Illness
Crohn’s can cause or worsen certain mental illnesses, especially depression and anxiety. One study found that instances of these disorders are highest within the first year of diagnosis.
These findings were in line with other research which “found depression and/or anxiety to be more common in patients with IBD than in the general population or in patient groups with other chronic diseases.”
Isolation And Loneliness
During an active state of Crohn’s, the unpredictability of the disease can make it difficult to socialize. A person with Crohn’s may feel so unwell, or grow to fear the onset of their symptoms and the difficulty of managing them, that they simply stay home.
To self-treat these states, a person may begin using drugs or alcohol, which can actually make these states more severe. As they worsen, a person may continue to drink or use drugs, to the point they become dependent and addicted to the substance.
How Are Crohn’s Disease And Substance Abuse Related?
Alcohol abuse is especially harmful to people with Crohn’s. It irritates an already inflamed digestive tract and increases the odds of further damage to these sensitive tissues.
Some research does show that marijuana may be helpful in treating certain symptoms of Crohn’s, but if a person self-treats their condition they do run the risk of becoming addicted.
Opioid painkillers may be used to treat the pain associated with Crohn’s or after surgery for the disease. But certain individuals may begin to use their medication improperly, which could lead to severe addiction.
What Factors Of An Addicted Lifestyle Can Aggravate Crohn’s?
The following lifestyle factors can aggravate Crohn’s Disease:
- Diet: Addicted individuals are more apt to make poor dietary choices, which are speculated to aggravate Crohn’s.
- Immune System: Substance abuse can decrease your immune system, which can trigger an episode, and make it harder for your body to fight Crohn’s.
- Smoking: Smoking makes Crohn’s disease worse. Certain forms of substance abuse, for instance alcohol, make certain people more apt to smoke.
- Stress: An addiction can destroy important aspects of your life such a your health, family, career, and educational pursuits. These happenings can increase stress which inflames Crohn’s.
Individualized Care Is Crucial When Treating Crohn’s Disease And Addiction
If you have Crohn’s disease and addiction, you need to ensure you’ll be in a treatment environment which is sensitive to the needs of both diseases (addiction is, itself, a disease).

Full-spectrum, individualized care is critical for patients who have both a chronic disease and addiction. Behavioral therapies, counseling, and other modalities should be adapted to help you heal on a physical, mental, emotional, and social level from both diseases.
Advanced Medical Care
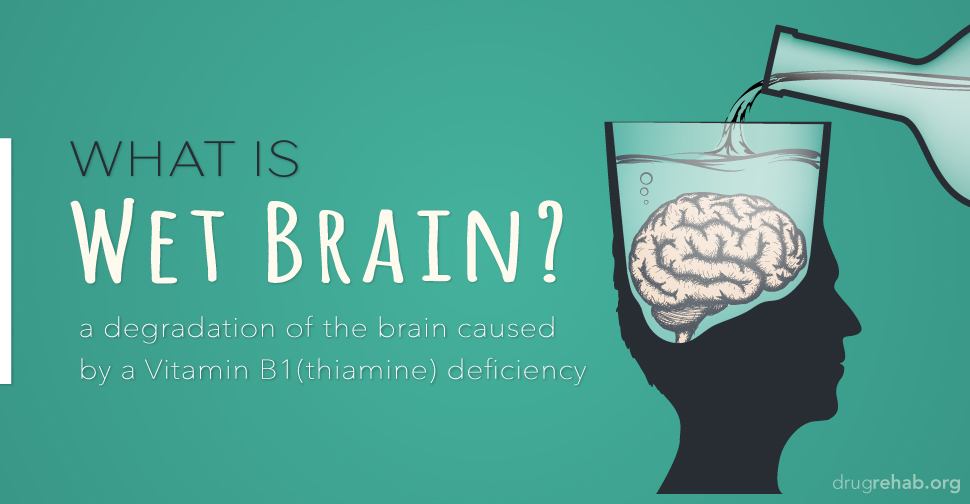
When the disease is an active state, you may require additional medical care, nutritive support, and even counseling. Certain B vitamins may be administered as they are used to treat both diseases.
Dual Diagnosis Care
Dual diagnosis care is an important element of treatment for those with a co-occurring mental health disorder. Non-addictive medications may be used to treat anxiety, depression, or any other mental illness which you suffer from.
Pain Management
For those in need of pain management, certain non-addictive medications or alternative therapies may be used.
Family Therapy And Support
Chronic disease and addiction can take an immense toll on your family members too. A comprehensive program should offer family therapy and support to help you grow and heal together within the face of such adversity.
Mindfulness And Stress Management Practices
Because stress can cause a flare-up of Crohn’s, it’s important to learn how to manage it in a healthy way. Mayo suggests the following techniques:
- Biofeedback
- Breathing exercises
- Meditation
- Yoga.
Many facilities offer these holistic therapies.
Fitness And Nutrition
A program may offer exercise facilities or classes which can help you to channel your stress in a healthful manner, all the while strengthening your body.
Even though experts are still learning about the role diet has on Crohn’s, it’s still important to be mindful of how you eat. A good facility will prepare meals which take into account any dietary restrictions you may have.
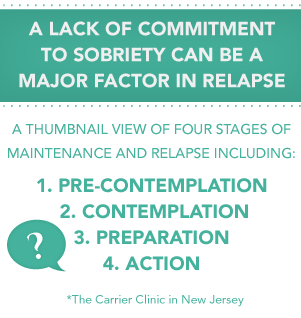
Relapse Prevention Training
Since Crohn’s is a lifelong disease, you must be prepared to deal with flare-ups, both mentally and physically. Without relapse prevention training, an active state could become a trigger for addiction. Enhanced coping skills will be taught to help you cope with these challenges.
Battling Crohn’s disease and addiction isn’t an easy task by any means, but it is possible to develop positive and healthy behaviors which can support a drug-free life and better overall physical health.
Even though there isn’t a cure for Crohn’s, the right combination of therapies can decrease the severity of symptoms and/or lead to long-term remission. Recovery from addiction is also something you need to commit to for life, but the right treatment program can make all the difference by preparing you for this journey.
Get Help For Chrohn’s Disease And Addiction Today
If you or a loved one has Crohn’s, you can still seek treatment. Protecting your body from the effects of drugs or alcohol is especially important with this concern, and DrugRehab.org wants to help you reach this goal. Contact us today to learn more about your treatment options.
For More Information Related to “Crohn’s Disease And Addiction” Be Sure To Check Out These Additional Resources From DrugRehab.org:
- Co-Occurring Disorders: Anxiety And Addiction
- Schizophrenia And Addiction
- Co-Occurring Disorders: Autism And Addiction
- Dual Diagnosis: Tourette’s Syndrome And Addiction
- Sensory Processing Disorder (SPD) And Addiction



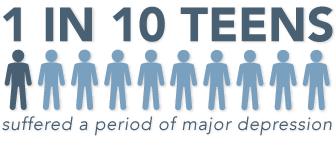
 There are a lot of different contributing factors leading to an addiction; these can be community, family, school, and friends (peers). Though not everyone who experiments with drugs becomes addicted, approximately
There are a lot of different contributing factors leading to an addiction; these can be community, family, school, and friends (peers). Though not everyone who experiments with drugs becomes addicted, approximately 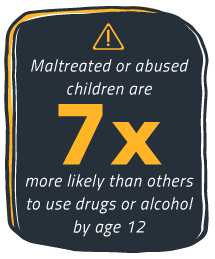 Teens will be exposed to drugs and alcohol, whether they’re the one using them or not. If they aren’t, it will be someone they know of who is using the drug. Scientists from the
Teens will be exposed to drugs and alcohol, whether they’re the one using them or not. If they aren’t, it will be someone they know of who is using the drug. Scientists from the  A person’s community can play a major role in their subjection to alcohol and drug addiction. “If a…community has favorable attitudes toward drug use, firearms and crime, their risk is increased.” (
A person’s community can play a major role in their subjection to alcohol and drug addiction. “If a…community has favorable attitudes toward drug use, firearms and crime, their risk is increased.” ( “The single biggest contributing factor to drug abuse risk is having friends who engage in the problem behavior.” (
“The single biggest contributing factor to drug abuse risk is having friends who engage in the problem behavior.” ( An adolescent’s first exposure to drug and alcohol use often takes place in the home–this usually depends on parenting practices and general home life. These risk factors are broken down into several categories, but two common understandings of child upbringing (as related to drug and alcohol use) are maltreatment and traumatic events. Parenting practices can play a significant role in substance use disorders and addiction. Sometimes, if a mom or dad is never around to see the sometimes obvious signs of drug and alcohol use, or neglect to educate their children–those same children can be at risk.
An adolescent’s first exposure to drug and alcohol use often takes place in the home–this usually depends on parenting practices and general home life. These risk factors are broken down into several categories, but two common understandings of child upbringing (as related to drug and alcohol use) are maltreatment and traumatic events. Parenting practices can play a significant role in substance use disorders and addiction. Sometimes, if a mom or dad is never around to see the sometimes obvious signs of drug and alcohol use, or neglect to educate their children–those same children can be at risk. Teen may be at risk for substance use and addiction when they miss out on extracurricular activities, or or when they lack some of the social structure that comes from good grades and commitment. People strive to fit in with whomever they surround them self with, these school mates might be involved in drugs (and who knows? Maybe there is an opportunity to help them out of it.), but when such an adolescent is surrounded by others who strive to do great things, they too will seek self-improvement and success.
Teen may be at risk for substance use and addiction when they miss out on extracurricular activities, or or when they lack some of the social structure that comes from good grades and commitment. People strive to fit in with whomever they surround them self with, these school mates might be involved in drugs (and who knows? Maybe there is an opportunity to help them out of it.), but when such an adolescent is surrounded by others who strive to do great things, they too will seek self-improvement and success.
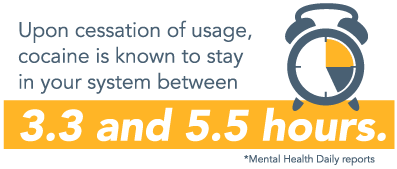
 Drug abuse has the potential to create numerous health effects, both physical and mental, within the lives of those who abuse. When a mental health disorder occurs with drug abuse, the two often worsen each other. Cocaine abuse, especially prolonged use, changes a person’s brain, affecting various chemical components, including certain important neurotransmitters which are critical within regulating a person’s mood. This effect may worsen existing depression or create new symptoms. Together, these disorders require effective substance abuse treatment.
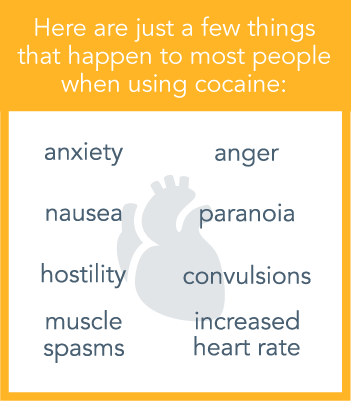
Drug abuse has the potential to create numerous health effects, both physical and mental, within the lives of those who abuse. When a mental health disorder occurs with drug abuse, the two often worsen each other. Cocaine abuse, especially prolonged use, changes a person’s brain, affecting various chemical components, including certain important neurotransmitters which are critical within regulating a person’s mood. This effect may worsen existing depression or create new symptoms. Together, these disorders require effective substance abuse treatment.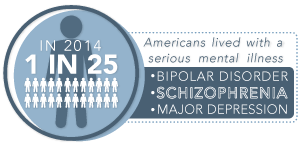 When using cocaine, there are several things which transpire concerning different aspects of the brain. Various neurotransmitters are affected, including the release of dopamine. When it comes to a sense of well-being, dopamine is the chemical which is considered to bring forth all kinds of pleasure and happy feelings. Dopamine releases when related to pleasure or a feeling of reward when it comes to specific activities in life. If dopamine levels become too high in the brain, they are linked to hallucinations, aggressiveness, delusions, anger, as well as other
When using cocaine, there are several things which transpire concerning different aspects of the brain. Various neurotransmitters are affected, including the release of dopamine. When it comes to a sense of well-being, dopamine is the chemical which is considered to bring forth all kinds of pleasure and happy feelings. Dopamine releases when related to pleasure or a feeling of reward when it comes to specific activities in life. If dopamine levels become too high in the brain, they are linked to hallucinations, aggressiveness, delusions, anger, as well as other 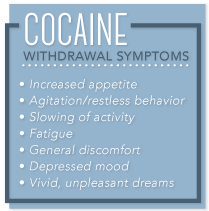 After extreme abuse over a period of time, stopping the use of cocaine can lead to cravings and depression for months. In some cases, suicidal thoughts may also occur. As someone faces withdrawal, the cravings grow more intense, even though the pleasurable effects of cocaine dip way down, instead becoming replaced by paranoia. When someone is facing withdrawal, here are some of the symptoms that may occur:
After extreme abuse over a period of time, stopping the use of cocaine can lead to cravings and depression for months. In some cases, suicidal thoughts may also occur. As someone faces withdrawal, the cravings grow more intense, even though the pleasurable effects of cocaine dip way down, instead becoming replaced by paranoia. When someone is facing withdrawal, here are some of the symptoms that may occur: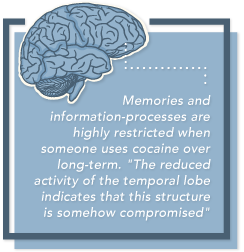 Memories and information-processes are highly restricted when someone uses cocaine over the long term. “The reduced activity of the temporal lobe indicates that this structure is somehow compromised,” says Dr. Nancy Pilotte of NIDA’s Division of Basic Neuroscience and Behavioral Research. “Some of these regions mediate the ability to connect emotionally, and cocaine’s blunting of them may induce a flattened affect similar to depression symptoms that are common among chronic cocaine abusers.”
Memories and information-processes are highly restricted when someone uses cocaine over the long term. “The reduced activity of the temporal lobe indicates that this structure is somehow compromised,” says Dr. Nancy Pilotte of NIDA’s Division of Basic Neuroscience and Behavioral Research. “Some of these regions mediate the ability to connect emotionally, and cocaine’s blunting of them may induce a flattened affect similar to depression symptoms that are common among chronic cocaine abusers.”
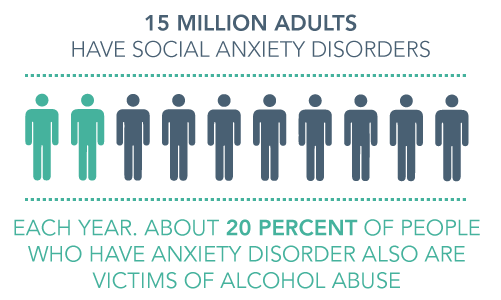
 Every little kid walks through a dark alley and gets the heebie jeebies, it’s just part of growing up. As they get older and recognize that there is no boogie man there to get them, they relinquish the fear and grow out of it. Some people go through life with that constant fear that something bad will happen. They very well could be suffering from a panic attack, which is defined by the
Every little kid walks through a dark alley and gets the heebie jeebies, it’s just part of growing up. As they get older and recognize that there is no boogie man there to get them, they relinquish the fear and grow out of it. Some people go through life with that constant fear that something bad will happen. They very well could be suffering from a panic attack, which is defined by the 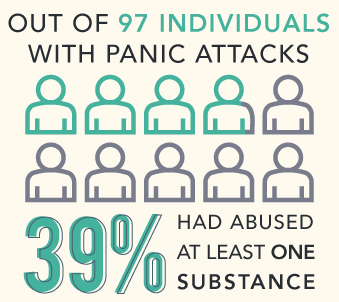 Not every substance will cause a panic attack, however, there are certain drugs that can. Some people suffering from a
Not every substance will cause a panic attack, however, there are certain drugs that can. Some people suffering from a  Caffeine is not always associated with substance abuse; however, it’s still a drug. When caffeine is consumed in heavy quantities, or more than a healthy amount, that’s abuse. Caffeine is a stimulant, and after it’s ingested (whether it’s in a pill form or in a beverage) it raises the heart rate. According to the
Caffeine is not always associated with substance abuse; however, it’s still a drug. When caffeine is consumed in heavy quantities, or more than a healthy amount, that’s abuse. Caffeine is a stimulant, and after it’s ingested (whether it’s in a pill form or in a beverage) it raises the heart rate. According to the  Alcohol is a drug which is sometimes referred to as “liquid courage”, because it can cause a person to do things that they might not normally do. Alcohol can lead to mood swings and temper tantrums–a person who abuses alcohol may exhibit bouts of rage, anxiety, and increased danger to his or herself and others. Withdrawal from alcohol can also lead to symptoms such as anxiety and panic attacks, but it can also lead to insomnia, delirium tremens, sweating profusely,
Alcohol is a drug which is sometimes referred to as “liquid courage”, because it can cause a person to do things that they might not normally do. Alcohol can lead to mood swings and temper tantrums–a person who abuses alcohol may exhibit bouts of rage, anxiety, and increased danger to his or herself and others. Withdrawal from alcohol can also lead to symptoms such as anxiety and panic attacks, but it can also lead to insomnia, delirium tremens, sweating profusely,  Marijuana can be smoked, consumed, or “dabbed”–the highest dose of tetrahydrocannabinol THC which can be abused. THC is the primary compound found in marijuana, and it can have serious affects on the mind of a person using it. Abuse of marijuana can lead to lack of motivation, mood swings, anxiety, and panic attacks. The
Marijuana can be smoked, consumed, or “dabbed”–the highest dose of tetrahydrocannabinol THC which can be abused. THC is the primary compound found in marijuana, and it can have serious affects on the mind of a person using it. Abuse of marijuana can lead to lack of motivation, mood swings, anxiety, and panic attacks. The 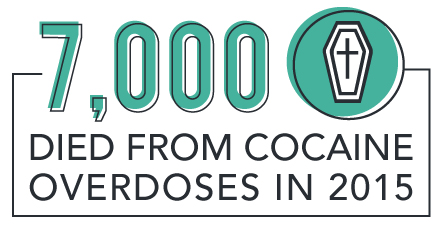
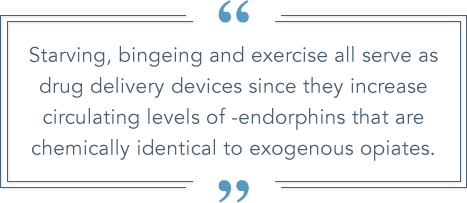
 Opioids such as heroin are characterized by spurts of intense euphoria and well-being. Abusing drugs like heroin can lead to anxiety, severe depression, and insomnia. Even after a person stops using opioids, the withdrawals can start after a couple hours and last for several weeks–withdrawal symptoms can be incredibly dangerous and sometimes include paranoia, anxiety, panic, and seizures. With the prolonged withdrawals associated with opioids, relapse is more likely to occur to avoid further withdrawals.
Opioids such as heroin are characterized by spurts of intense euphoria and well-being. Abusing drugs like heroin can lead to anxiety, severe depression, and insomnia. Even after a person stops using opioids, the withdrawals can start after a couple hours and last for several weeks–withdrawal symptoms can be incredibly dangerous and sometimes include paranoia, anxiety, panic, and seizures. With the prolonged withdrawals associated with opioids, relapse is more likely to occur to avoid further withdrawals. Hallucinogens can give the user visual and mental delusions–or hallucinations. A person who is abusing hallucinogens (such as LSD, Peyote, PCP, and Psilocybin Mushrooms (or Shrooms)) can become dangerously antisocial. They might experience bouts of laughter, which can be followed by unexplainable crying. A person using these kind of drugs can very quickly slip into a drug induced panic attack, or lapse into paranoia. Withdrawal from some hallucinogens can be feeling of emptiness, prolonged trip (or “permi-trip”), inability to eat, anxiety, and fatigue.
Hallucinogens can give the user visual and mental delusions–or hallucinations. A person who is abusing hallucinogens (such as LSD, Peyote, PCP, and Psilocybin Mushrooms (or Shrooms)) can become dangerously antisocial. They might experience bouts of laughter, which can be followed by unexplainable crying. A person using these kind of drugs can very quickly slip into a drug induced panic attack, or lapse into paranoia. Withdrawal from some hallucinogens can be feeling of emptiness, prolonged trip (or “permi-trip”), inability to eat, anxiety, and fatigue.
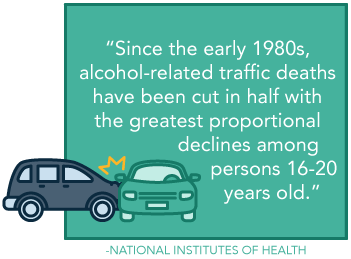 Despite its legal standing, prevalence, and acceptance within numerous social spheres, alcohol is not a benign drug. One of the most common and destructive ways in which this occurs is within circumstances regarding an individual driving after they have been drinking. In decades past, this behavior was more commonplace and even somewhat socially acceptable. Fortunately now, with the advent of more strident rules and social perspectives, this behavior has declined, as evidenced, in part, by statistics presented by the
Despite its legal standing, prevalence, and acceptance within numerous social spheres, alcohol is not a benign drug. One of the most common and destructive ways in which this occurs is within circumstances regarding an individual driving after they have been drinking. In decades past, this behavior was more commonplace and even somewhat socially acceptable. Fortunately now, with the advent of more strident rules and social perspectives, this behavior has declined, as evidenced, in part, by statistics presented by the 
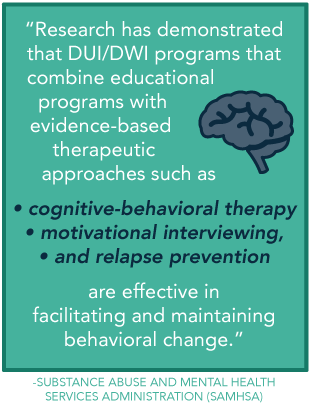 Yes. While you will likely be able to choose most any program, there are certain programs that are especially designed for DUI/DWI offenders. According to the Substance Abuse and Mental Health Services Administration (SAMHSA) “
Yes. While you will likely be able to choose most any program, there are certain programs that are especially designed for DUI/DWI offenders. According to the Substance Abuse and Mental Health Services Administration (SAMHSA) “
 Narcissism is rarely a desired attribute, though it is often directly related to a personality disorder. Personality disorders fall into the
Narcissism is rarely a desired attribute, though it is often directly related to a personality disorder. Personality disorders fall into the 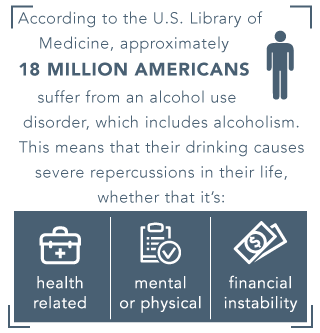 According to the
According to the  A person who is suffering from alcoholism and narcissistic personality disorder, might answer the question (How the heck aren’t you drunk yet?), with a false sense of pride or by stating anything other than “because I can’t stop drinking”, or by stating, “I have built up a tolerance.” There are many accomplishments that deserve a person the right to be proud of themselves, but unfortunately, alcoholism is not one of them, and it’s dangerous to believe that it is. Intervention and treatment are very likely the only way to get a person on the right track towards recovery. Try to remember that Alcoholism is a disease and the person with it is very sick.
A person who is suffering from alcoholism and narcissistic personality disorder, might answer the question (How the heck aren’t you drunk yet?), with a false sense of pride or by stating anything other than “because I can’t stop drinking”, or by stating, “I have built up a tolerance.” There are many accomplishments that deserve a person the right to be proud of themselves, but unfortunately, alcoholism is not one of them, and it’s dangerous to believe that it is. Intervention and treatment are very likely the only way to get a person on the right track towards recovery. Try to remember that Alcoholism is a disease and the person with it is very sick.
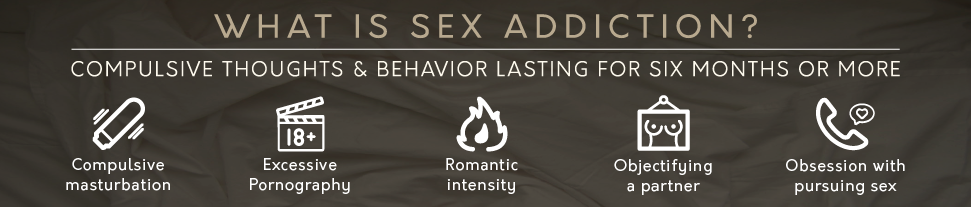
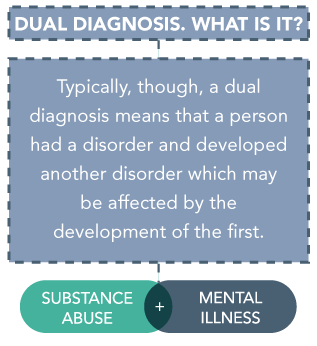 People affected by dual diagnosis may experience dire effects to their health; each disease can greatly influence the other, and either disease can occur first. Further, the problem of dual diagnosis is vast. As NAMI reports, “about a third of all people experiencing mental illnesses and about half of people living with severe mental illnesses also experience substance abuse.” The reverse is also true, as nearly the same amount of people affected by substance abuse are suffering from mental illness as well.
People affected by dual diagnosis may experience dire effects to their health; each disease can greatly influence the other, and either disease can occur first. Further, the problem of dual diagnosis is vast. As NAMI reports, “about a third of all people experiencing mental illnesses and about half of people living with severe mental illnesses also experience substance abuse.” The reverse is also true, as nearly the same amount of people affected by substance abuse are suffering from mental illness as well. Symptoms of mental illness are great in number, but some may signal the development of a disorder. A person with a developing mental illness may have problems concentrating at school or work, undergo severe mood changes, withdraw from family or friends, or have
Symptoms of mental illness are great in number, but some may signal the development of a disorder. A person with a developing mental illness may have problems concentrating at school or work, undergo severe mood changes, withdraw from family or friends, or have  Some of the best treatments can occur in an
Some of the best treatments can occur in an 



 One of the biggest changes between the DSM-IV and DSM-V criteria, is the
One of the biggest changes between the DSM-IV and DSM-V criteria, is the