We welcome them home. We cry. We laugh. But underneath the surface, do we truly understand the struggle the U.S. veteran experiences? Our U.S. military veterans are extraordinary individuals who have faced extreme emotional and mental challenges from what they’ve seen, heard, and felt, during their time in the United States Armed Forces.
Many Experience Trauma
After deployment, these individuals often face traumatic experiences which creates an aftermath of devastating effects. If not properly cared for, these may lead to many other concerns such as homelessness, mental health problems, suicide, alcoholism, and drug abuse. Fighting for our country, these men and women have braved numerous obstacles, only to come back to a world that may seem foreign to them. Feeling out of touch with their former way of life and loved ones, it might be difficult for them to grasp what they went through.
With trauma buried deep inside, these individuals often times don’t know how to cope or recover from the difficult sights they witnessed during their time in the service. With posttraumatic stress disorder (PTSD), mental issues, and physical strain, many veterans fight this inner battle on a daily basis. Some, unfortunately, don’t seek or receive the proper care they so desperately need. The need to be able to survive their daily lives starts to snowball, and without the proper treatment a veteran might reach out for any means of escape from the mental, emotional, and physical pain that plagues their daily lives. Too often this desire to self-medicate leads them to drugs or alcohol, a long and dangerous path.
Homelessness In Our Veterans
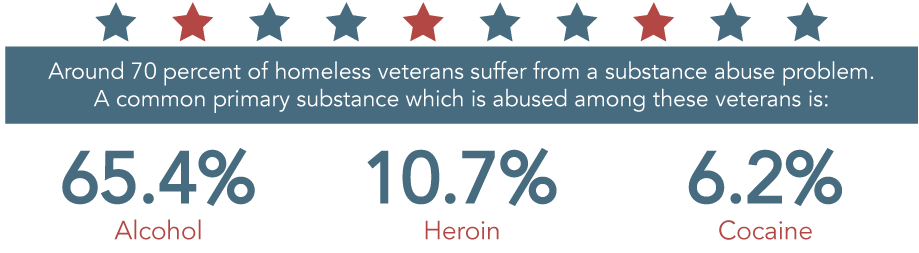
The unfortunate truth is that a large amount of our veterans become homeless. With military conflicts on the rise, there is also a high possibility that the number will continue to increase. One of the difficulties a homeless veteran encounters is substance abuse. Around 70% of homeless veterans suffer from a substance abuse problem. A common primary substance which is abused among these veterans is alcohol (65.4 %), followed up by heroin (10.7%), and cocaine (6.2 %).
Mental Health Issues Lead To More Concerns
Mental health issues are a rising concern amongst these brave individuals. Another study showed that 20% of active duty and 42% of reserve soldiers were in need of mental health treatment. Frequent use of drugs or alcohol were often associated with mental health problems.
The National Institute on Drug Abuse cites that one in four veterans who returned from Iraq and Afghanistan were reported to have symptoms of mental or cognitive problems, while one in six exhibited signs of PTSD. Substance abuse and dependance go hand-in-hand with these mental disorders, as well as trauma to the brain, sleep problems, and exhibiting violent behavior in relationships.

Younger veterans are a much greater risk to have substance abuse issues or mental health problems. NIDA further elaborates, stating that of those veterans aged 18-25, a quarter qualified as having a past-year substance use disorder. To further put this in perspective, they noted that this is double the prevalence of those aged 26-54, and five times that of veterans who are 55 and beyond.
Suicide And Substance Abuse
In January 2014, the Veterans Health Administration reported that the suicide rates between male and female veterans and military service members outweighed the overall rate of the general population. With 20% of all national suicides, a startling 22 veterans are committing suicide every day.
There are often underlying mental or substance use disorders affecting these individuals. Research presented by the U.S. National Library of Medicine supports this, noting that within the study’s veteran cohort, “There was a high prevalence of diagnosed alcohol disorder or abuse (31.8%), drug dependence or abuse (21.8%), psychoses (21.2%), depression (18.5%)….” Certain findings suggest that 45 percent of nonfatal suicide attempts of suicide involved mental health issues mixed with substance abuse. Other reports cite that three out of the five veterans who committed suicide had been diagnosed with a mental health condition.
The Alcohol Problem
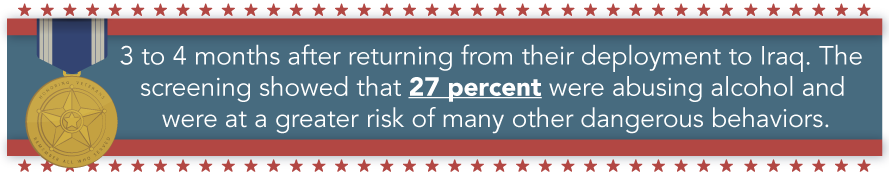
A group of army soldiers went through a screening process 3 to 4 months after returning from their deployment to Iraq. The screening showed that 27% were abusing alcohol and were at a greater risk of many other dangerous behaviors, including drinking and driving, and using illicit drugs. Even after soldiers have been reported for alcohol issues, there are few who are referred to alcohol treatment programs. The increasing need for improvement with screenings and access to care for alcohol-related problems, among veterans, is highly needed for those coming back from combat deployments.
Prescription Drug Abuse
Individuals who have been deployed several times, exposing them to multiple combat situations, and other related injuries are a higher risk of developing substance abuse issues. The risk of heavy drinking, binge drinking, smoking, or a relapse to smoking are prominent in these veterans. However, perhaps the greatest concern is prescription drug abuse. Veterans, like civilians, are at risk for addiction to opioid pain medicines that were prescribed due to combat-related injuries.
A special report for the United States Senate Committee on Veterans’ Affairs notes that in comparison to the 30% of the general population that suffer from chronic pain, 60% of veterans from deployments in the Middle East, and 50% of older veterans struggle with this condition.
This is not without repercussions. Due to the prevalence of chronic pain within the veteran population, prescriptions for opioid painkillers are increasingly more common. According to study findings published by the U.S. National of Library Medicine, in comparison to the general population, Veterans Health Administration patients encountered roughly double the number of accidental poisonings, most notably with cocaine and opioid medications.
Frontline news reports that in five years, from 2010 to 2015, opioid-use disorders have skyrocketed 55% within the veteran population. They continue to say that 13% of those veterans that receive opioid medications experience these disorders.
How Can We help?
Understanding the health and mental needs of a veteran is gravely important to the friends, family, and community of these individuals. Becoming aware, having compassion, and reaching out for proper help for your loved ones is key to bringing healing to those who are suffering from these illnesses.
 If you or a loved one has experienced traumatic experiences or substance use disorders, reach out today. Proper and compassionate care is highly needed to help you overcome these struggles. Let us be the helping hand you need to overcome these obstacles. Contact us today.
If you or a loved one has experienced traumatic experiences or substance use disorders, reach out today. Proper and compassionate care is highly needed to help you overcome these struggles. Let us be the helping hand you need to overcome these obstacles. Contact us today.
Sources
Substance Abuse and Mental Health Services Administration — The TEDS Report: Twenty-one Percent of Veterans in Substance Abuse Treatment Were Homeless
Substance Abuse and Mental Health Services Administration — The CBHSQ Report: Veterans’ Primary Substance of Abuse is Alcohol in Treatment Admissions
National Institute on Drug Abuse — Drug Facts–Substance Abuse in the Military
U.S. National Library of Medicine — Suicide among War Veterans