When methamphetamine-associated psychosis (MAP) occurs in a loved one, it can be a frightening thing to behold. It will change their behavior in negative ways and can make them unpredictable. Understanding the signs of methamphetamine psychosis can help you to know what to look for in your loved one and to get them immediate treatment.
Effects Of Methamphetamine On The Body And Mind
Methamphetamine causes a variety of severe and negative short and long-term effects on the mind and body, some of which may contribute to methamphetamine psychosis onset. Meth can also cause a variety of mental health problems including irritation, nervousness, tremors, anxiety, paranoia, aggressiveness, and confusion.
Even in the short-term, meth suppresses systems that are crucial for health and survival. According to Arizona State University, “Meth also effectively shuts down your brain’s sleep, hunger, and thirst centers.” With continued use, these short-term effects can worsen and can grow into more damaging long-term effects.
Long-term effects include severe heart problems (irregular heart beat, damage to blood vessels, stroke, etc.), abscesses in the skin, osteoporosis, problems with libido, the sensation of insects under the skin, the need for an increasing dosage as tolerance increases in order to simulate the original high, and neurological damage that can cause mood disturbances, delusions, and paranoid thoughts.
Unfortunately, it is possible for these neurological symptoms to coalesce into methamphetamine psychosis. Understanding the symptoms specific to this disorder is crucial to helping your loved one beat this condition.
The Signs And Symptoms Of Methamphetamine Psychosis
Methamphetamine psychosis is a non-schizophrenic mental disturbance that creates a series of dangerous false perceptions. The most common of these are  hallucinations, including:
hallucinations, including:
- Auditory (hearing noises that aren’t made, such as voices giving commands)
- Visual (seeing things that aren’t there, such as a person staring from across the room)
 Olfactory (odors that don’t exist, such as the smell of rotting flesh)
Olfactory (odors that don’t exist, such as the smell of rotting flesh)- Tactile (feeling something on the skin that isn’t there, like bugs or insects)
- Gustatory (tasting something false, such as a poison in all food)
 Delusions are another common symptom of methamphetamine psychosis. Delusions are false beliefs that don’t coincide with reality. Common delusions include persecution (being pursued by higher authorities), grandeur (feeling important or powerful), references (connecting random events to their lives), control (people are manipulating behaviors),
Delusions are another common symptom of methamphetamine psychosis. Delusions are false beliefs that don’t coincide with reality. Common delusions include persecution (being pursued by higher authorities), grandeur (feeling important or powerful), references (connecting random events to their lives), control (people are manipulating behaviors),
and somatic (parts of the body are changing).
These delusions can fuel paranoia about the world, such as the belief that a random surveillance camera was installed to monitor a person’s behavior. This can also lead to various obsessions, including compulsive actions, manifestations, and beliefs, such as regularly showering, hoarding strange items, and following a strict path from work to home to evade dangerous people or events.
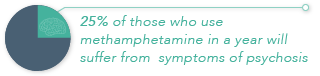
Symptoms like these can be difficult to manage and are prominent with methamphetamine use. One estimate claims that nearly 25 percent of those who use methamphetamine in a year will suffer from symptoms of psychosis. The study pointed out that dependence of methamphetamine was key to this increased risk.
Another possible connection in the development of this problem was a history of schizophrenia, while methamphetamine psychosis can manifest itself in a person without schizophrenia, it may adversely affect a person that has it. A study published by the Journal of Neuroimmune Pharmacology, noted this connection, stating “While amphetamines such as METH can precipitate and exacerbate psychotic symptoms in persons with schizophrenia, it has long been recognized that such drug use can produce psychotic symptoms even in persons with no history of a primary psychotic disorder.”
The Connection With Schizophrenia
If methamphetamine psychosis is not the same as schizophrenia, what is the connection between these two problems? The connection may lie in the way both influence dopamine release. A study published by The American Journal Of Psychiatry stated in its conclusion:
“…longer use of methamphetamine may cause more severe psychiatric symptoms and greater reduction of dopamine transporter density in the brain. They also show that the dopamine transporter reduction may be long-lasting, even if methamphetamine use ceases. Further, persistent psychiatric symptoms in methamphetamine users, including psychotic symptoms, may be attributable to the reduction of dopamine transporter density.”
Beyond dopamine release was the connection noted in the study “Determining Vulnerability To Schizophrenia In Methamphetamine Psychosis Using Exploratory Eye Movements,” which stated: “This finding suggests that there is a possibility that the patients of MAP psychosis include a few who have a vulnerability to schizophrenia.” This report seems to indicate that methamphetamine psychosis is a potent risk for those who suffer from schizophrenia.
Another study indicated that heavy methamphetamine psychosis may, in some cases, merely mimic its symptoms, while in others, the pre-morbid condition may put a person at greater risk. The study, “Pre-Morbid Characteristics And Co-Morbidity Of Methamphetamine Users With And Without Psychosis,” published by the Cambridge University Press, concluded that “The MAMP users with psychosis presented a clinical picture which mimicked the positive symptoms of schizophrenia: 85% had auditory hallucinations; 71% persecutory delusions; 63% delusions of reference.” They acknowleged other research findings, citing that “Our data are also compatible with the view that pre-morbid schizoid/schizotypal personality predisposes MAMP users to develop psychosis, and that the greater the personality vulnerability, the longer the psychosis will persist.”
Within the last study, psychosis of this type was more noticeable in those who had used methamphetamine from a younger age and at larger doses. That’s why it is so important to treat methamphetamine psychosis as soon as symptoms appear. The treatment methods for this problem vary on a case-by-case basis, but follow similar protocols.
Treating Methamphetamine Psychosis
When methamphetamine psychosis occurs, it is important to manage its symptoms immediately to decrease their severity. The American College of Emergency Physicians created a series of important suggestions for the instances of an “acutely agitated patient in the ED,” which have guided the treatment of methamphetamine psychosis and helped decrease its severity. These recommendations include:
- Using a conventional anti-psychotic, specifically, droperidol and haloperidol, with the former being used in cases of quick sedation (which may be necessary if behavior puts their life or the lives of others at risk)
- Managing agitation with typical or atypical anti-psychotics if any known psychiatric illness is present
- Implementing oral benzodiazepine and risperidone for those who are agitated, but willing to cooperate
- Combining parenteral benzodiazepine and haloperidol for very quick sedation in those who are very agitated and uncontrollable
The idea of these guidelines is to help health care specialists understand proper behavior and treatment methods in what can be a scary situation. These medicines are designed to calm the symptoms of psychosis and create a more focused and clear-headed state. In some instances, clozapine may be used for those who don’t react to these medicines.
Once the person who suffered from methamphetamine psychosis is calm and has recovered sufficiently, it is important to get them rehabilitation treatment. This can help them beat addiction to methamphetamine and regain a sober life.
Managing Methamphetamine Addiction
After methamphetamine psychosis has been successfully treated, the symptoms of addiction must be managed. Withdrawal from methamphetamine can be physically dangerous and severe, which is why a variety of medicines are being tested as a method for treating withdrawal. Some of these medicines include:
- Buproprion
- Naltrexone
- Modafinil
- Mirtazapine
- Rivastigmine
- Topiramate
- Dextroamphetamine
- Nicotine
These medicines may help reduce cravings and methamphetamine use. Most of them are still being tested for efficiency, but it is possible to receive them at some rehab centers. In this way, detoxification is easier to handle and the body is cleaned of all addictive substances to improve physical and mental health.
After detoxification is finished, psychotherapy techniques are utilized. These methods (such as individual therapy, group meetings, and intensive family sessions) identify underlying issues that contribute to addiction and find a treatment method to help decrease their severity. By breaking up co-occurring disorders, it is possible to get a new start on the road to recovery.
 Though psychotherapy takes up a large part of treatment, behavior-modification techniques will also be implemented. These will not only help correct negative behavior patterns that contribute to methamphetamine use, but also manage negative side effects, such as itching skin. It can also help manage any relapse cravings and help to alleviate early psychosis warning signs.
Though psychotherapy takes up a large part of treatment, behavior-modification techniques will also be implemented. These will not only help correct negative behavior patterns that contribute to methamphetamine use, but also manage negative side effects, such as itching skin. It can also help manage any relapse cravings and help to alleviate early psychosis warning signs.
Treatment like this is designed to help not only beat methamphetamine addiction, but to decrease the recurrence of psychosis. It can be obtained in various rehab centers around the nation, including ones that may be close to your home town.
Find The Help You Need
 If you are looking for help for someone with a methamphetamine addiction, our experts at DrugRehab.org can point you in the right direction. They have years of experience helping people find powerful recovery resources and want to help you in the fight against addiction. Please contact us today.
If you are looking for help for someone with a methamphetamine addiction, our experts at DrugRehab.org can point you in the right direction. They have years of experience helping people find powerful recovery resources and want to help you in the fight against addiction. Please contact us today.
Sources
Arizona State University – What Does Methamphetamine Do To Your Body?
The American Journal Of Psychiatry – Methamphetamine-Related Psychiatric Symptoms And Reduced Brain Dopamine Transporters Studied With PET
Psychiatry And Clinical Neurosciences – Determining Vulnerability To Schizophrenia In Methamphetamine Psychosis Using Exploratory Eye Movements
Cambridge Journals – Pre-morbid Characteristics and Co-morbidity of Methamphetamine Users With and Without Psychosis
American College of Emergency Physicians – Critical Issues in the Diagnosis and Management of the Adult Psychiatric Patient in the Emergency Department
Hindawai Publishing Corporation – Treating Methamphetamine-Induced Resistant Psychosis With Clozapine
The Journal of Neuropsychiatry And Clinical Neurosciences – Neuropsychological Effects of Chronic Methamphetamine Use on Neurotransmitters and Cognition: A Review
National Center For Biotechnology Information – Symptoms and Course Of Psychosis After Methamphetamine Abuse: One-Year Follow-Up Of A Case
National Center For Biotechnology Information – Methamphetamine-Associated Psychosis


 “The comorbid presentation of PTSD and SUDs is remarkably common, and in comparison to patients presenting with either PTSD or SUD alone, PTSD/SUD patients often report greater functional impairment and experience poorer treatment outcomes –including treatment failure and dropout. Several mechanisms have been posited to explain the co-occurrence of PTSD and SUDs, including the self-medication hypothesis, the high-risk hypothesis, the susceptibility hypothesis. The majority of research to date supports the self-medication hypothesis.”
“The comorbid presentation of PTSD and SUDs is remarkably common, and in comparison to patients presenting with either PTSD or SUD alone, PTSD/SUD patients often report greater functional impairment and experience poorer treatment outcomes –including treatment failure and dropout. Several mechanisms have been posited to explain the co-occurrence of PTSD and SUDs, including the self-medication hypothesis, the high-risk hypothesis, the susceptibility hypothesis. The majority of research to date supports the self-medication hypothesis.”