The United States is currently in the midst of an opioid crisis, but determining which opioids are the biggest problem can be difficult. Opioids include illicit drugs like heroin, and powerful pain relieving medications like oxycodone, and methadone. Even though they share the same classification, methadone and oxycodone have many differences.
Methadone Vs. Oxycodone
Most opioids have potential to produce a high and can lead to addiction, but some are more powerful than others.
Even though the drug excites the same opioid receptors in the brain as oxycodone, methadone is not derived from opium. Nonetheless, both oxycodone and methadone are central nervous system depressants that can be used to decrease the amount of pain perceived by a patient.

Opioids can be naturally derived from the opium poppy plant; semi-synthetic, or derived from natural opioids and mixed with other chemicals; or fully synthetic and completely man made. Methadone is a fully synthetic opioid, and has a much longer half-life than oxycodone, which is a semi-synthetic opiate.
You won’t feel the effects of methadone as quickly, but it’s still effective—it just takes longer to activate in your system. Methadone can also take longer to leave the system.
There are three different types of opioids, as reported by the National Institute On Drug Abuse (NIDA) for Teens:
- Natural opiates are alkaloids, nitrogen-containing base chemical compounds that occur in plants such as the opium poppy. Natural opiates include morphine, codeine, and thebaine.
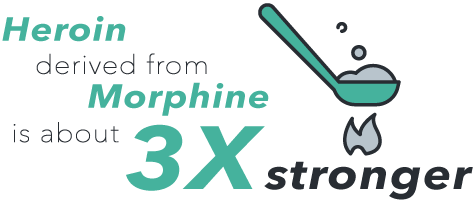
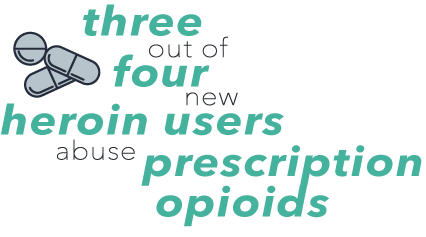
- Semi-synthetic/man-made opioids are created in labs from natural opiates. Semi-synthetic opioids include hydromorphone, hydrocodone, and oxycodone (the prescription drug OxyContin), as well as heroin, which is made from morphine.
- Fully synthetic/manmade opioids are completely man-made, including fentanyl, pethidine, levorphanol, methadone, tramadol, and dextropropoxyphene.
Why Is Methadone Used Instead Of Oxycodone?
Methadone has a longer half-life and less potential for abuse. Because of this, methadone may be offered in a clinical setting to replace the effects of, or help to avoid withdrawal symptoms caused by, oxycodone, morphine, hydrocodone, or heroin.
Methadone can also be helpful for pain management for someone suffering from an addiction to oxycodone, or from natural or other semi-synthetic opiates. Methadone can still be abused for the euphoric effect, when someone tampers with the dose size, frequency, or method of administration.
The half-life of methadone can be anywhere from 24 to 60 hours, so it can help prevent opioid withdrawal symptoms for a full day. At the same time, the effects of methadone aren’t achieved as quickly as the effects of oxycodone, which has a half-life of about four hours and rapidly takes effect.

To find out the appropriate dose size, it’s vital to speak to a doctor before deciding to take more of a drug. The potency for an opioid is measured in comparison to morphine. This is known as the MME, or morphine milligram equivalent, and doses are regulated on a daily milligram measurement.
The MME for 50 mg per day of oxycodone is 33 mg (~2 tablets of oxycodone sustained-release 15 mg), and 12 mg of methadone ( <3 tablets of methadone 5 mg).
“Calculating the total daily dose of opioids helps identify patients who may benefit from closer monitoring, reduction or tapering of opioids, prescribing of naloxone, or other measures to reduce risk of overdose,” according to the Center for Disease Control and Prevention (CDC).
Methadone is also a cheaper alternative to oxycodone. When a patient’s health insurance contribution has run out for the year, they become responsible for paying for their meds out of pocket. This is why a lot of people switch to methadone, because they are unable to pay for expensive prescriptions like OxyContin.
What Are The Overdose Rates And Risks Of Methadone And Oxycodone?
Both methadone and oxycodone are large contributors to the United States opioid epidemic. “From 2000 to 2015 more than half a million people died from drug overdoses. Ninety-one Americans die every day from an opioid overdose,” the Center for Disease Control and Prevention reports.
Because oxycodone is more potent than methadone, doctors prescribe smaller doses of it and monitor patients to avoid overdose. Methadone can also result in overdose. However, due to successful monitoring and use, the rate has substantially decreased since 1999. “The rate of methadone overdose deaths increased 600%, from 0.3 persons per 100,000 in 1999 (784) to 1.8 in 2006 (5,406), was stable in 2007 (5,518), and then declined 39% to 1.1 (3,400) in 2014,”s as reported by the CDC.

Nearly half of the opioid overdoses in the United States involve a prescription opioid. In 2015, more than 15,000 people died from overdoses involving prescription opioids. The top three contributors to those deaths were oxycodone (OxyContin), hydrocodone (Vicodin), and methadone.
Not everyone who overdoses on opioids purposely abuses the drug. These adverse consequences can happen just as easily when a person who uses an opioid for a medical purpose increases the dose size. Some people decide that an opioid isn’t working, or no longer feel the effects due to tolerance, so they take more. This is especially true of methadone because of the prolonged activation time.
Taking too much of any opioid highly increases the chances of overdose. Overdose occurs when a dose size exceeds the amount that the body is able to metabolize. It can result in coma, respiratory failure, and death.
It’s vitally important to pay attention to dose sizes of both methadone and oxycodone. But overdose isn’t the only risk of abusing these drugs. They can also result in serious addiction, dependence, long-term health consequences, and other injuries such as:
- In 2014, almost 2 million Americans abused or were dependent on prescription opioids.
- As many as one in four people who receive prescription opioids long-term for noncancerous pain in primary care settings struggles with addiction.
- Every day, over 1,000 people are treated in emergency departments for misusing prescription opioids.
- In 2009, opioids were the cause of more than 475,000 emergency room visits.
Opioid Addiction Treatment
Opioid addiction and dependence may require a medically-supervised detox to overcome the physical addiction (dependence). Detoxification may be necessary when a person stops using opioids because managing withdrawal symptoms can be life-threatening and dangerous
After detox, a lot of patients benefit from behavioral treatment to overcome the mental addiction. During a behavioral treatment program, clients learn healthy coping skills, healthy reactions, and ways to adapt to their surroundings. They also learn relapse prevention skills, positive thinking and behaviors, as well as learn to love themselves again. Addiction treatment programs can be conducted in an inpatient rehab center, or other clinical environments that contribute to a healthy lifestyle.
In some cases, a medication will be helpful to manage withdrawal, which can be one of the hardest parts of recovery, and when relapse is the most frequent. A medication-assisted treatment may include methadone maintenance for oxycodone, or other semi-synthetic opiates. Other types of opioid medication-assisted treatment may include naloxone, or buprenorphine (or a mixture of both—Suboxone or Subutex).
Some of the best behavioral treatment modalities for an opioid addiction are cognitive behavioral therapy, dialectical behavioral therapy, or motivational interviewing. There are a lot of different phases of recovery. Admitting there’s a problem is often the first step, but that isn’t always easy. Sometimes asking for help is the best way to overcome the first hurdle of recovery.
Choosing The Right Rehab Center For Opioids
Contact DrugRehab.org today to speak to someone who can find the right treatment program for you or your loved one. All calls are 100 percent confidential.
For More Information Related to “What Is The Difference Between Methadone And Oxycodone?” Be Sure To Check Out These Additional Resources From DrugRehab.org:
- Long-Term Effects Of Taking Methadone
- Consequences Of Injecting OxyContin (Oxycodone)
- Gray Death Heroin Abuse In The United States
- The Dangers of Mixing Xanax and Oxycodone
- A Quantum Leap in Pain Relief?
Sources
Center for Disease Control and Prevention—Calculating Total Daily Dose Of Opioids For Safer Dosage, Methadone Prescribing and Overdose and the Association with Medicaid Preferred Drug List Policies, Understanding the Epidemic: Drug Overdose
NIDA for Teens – What Are the Different Types of Opioids?



 One of the first signs of cocaine use will appear when an individual runs out of money. Cocaine is one of the more expensive drugs, and the high from it doesn’t last very long so one binge can be costly. According to the
One of the first signs of cocaine use will appear when an individual runs out of money. Cocaine is one of the more expensive drugs, and the high from it doesn’t last very long so one binge can be costly. According to the  Someone using cocaine might stay up later than usual, sleep at odd times during the day, spend a lot of time alone, and excessively use the bathroom without good reason. Suspicious activities may also include anonymous phone calls, and when
Someone using cocaine might stay up later than usual, sleep at odd times during the day, spend a lot of time alone, and excessively use the bathroom without good reason. Suspicious activities may also include anonymous phone calls, and when  Sometimes the physical changes from cocaine use are the last thing people notice before they realize it’s a problem. Using cocaine temporarily decreases a person’s need for food and sleep. So as a result, they may lose a lot of weight, or even seem gaunt, or malnourished. Cocaine use may also come with the appearance of dark circles around the eyes.
Sometimes the physical changes from cocaine use are the last thing people notice before they realize it’s a problem. Using cocaine temporarily decreases a person’s need for food and sleep. So as a result, they may lose a lot of weight, or even seem gaunt, or malnourished. Cocaine use may also come with the appearance of dark circles around the eyes. 
 This is only a potential scenario, and doesn’t apply to everyone—the point is that though not everyone abuses prescription drugs for the same reason, all of our minds are wired the same way to crave things that make us feel good.
This is only a potential scenario, and doesn’t apply to everyone—the point is that though not everyone abuses prescription drugs for the same reason, all of our minds are wired the same way to crave things that make us feel good.


 Ativan is a brand name medication of the benzodiazepine (benzo) drug lorazepam. As a benzo, it’s a central nervous system (CNS) depressant, which means it slows several important bodily functions, including breathing rates, heart rate, and temperature. The
Ativan is a brand name medication of the benzodiazepine (benzo) drug lorazepam. As a benzo, it’s a central nervous system (CNS) depressant, which means it slows several important bodily functions, including breathing rates, heart rate, and temperature. The 
 Detox can be emotionally strenuous as well, which is another reason detoxing in a facility is so important. The facility’s staff will comfort you during this time, answering any questions you may have, or will simply provide an ear and any emotional support you may need.
Detox can be emotionally strenuous as well, which is another reason detoxing in a facility is so important. The facility’s staff will comfort you during this time, answering any questions you may have, or will simply provide an ear and any emotional support you may need.

 When used as a medical treatment, the prescribing doctor should gradually taper you off of the drug as to avoid unpleasant side effects of withdrawal. These professionals are trained and understand how to best do this to avoid any complications and further strain to your physical and mental states.
When used as a medical treatment, the prescribing doctor should gradually taper you off of the drug as to avoid unpleasant side effects of withdrawal. These professionals are trained and understand how to best do this to avoid any complications and further strain to your physical and mental states.




 Codeine has been mixed with different drugs to treat various medical conditions, most commonly acetaminophen. There are various strengths of this drug combination, indicated in the title of the drug as Tylenol 2, Tylenol 3, and Tylenol 4. Tylenol 4 is the most potent of these medications, containing 60mg of codeine and 325mg of acetaminophen.
Codeine has been mixed with different drugs to treat various medical conditions, most commonly acetaminophen. There are various strengths of this drug combination, indicated in the title of the drug as Tylenol 2, Tylenol 3, and Tylenol 4. Tylenol 4 is the most potent of these medications, containing 60mg of codeine and 325mg of acetaminophen. While reducing the amount and frequency of opioids if you have a substance abuse issue is important, quitting abruptly can be extremely dangerous. Because your brain has become accustomed to a certain level of opioids binding with your opioid receptors, your body considers this new chemical balance to be the norm. If you suddenly stop taking opioids, then this level will come down too rapidly, resulting in withdrawal symptoms.
While reducing the amount and frequency of opioids if you have a substance abuse issue is important, quitting abruptly can be extremely dangerous. Because your brain has become accustomed to a certain level of opioids binding with your opioid receptors, your body considers this new chemical balance to be the norm. If you suddenly stop taking opioids, then this level will come down too rapidly, resulting in withdrawal symptoms.
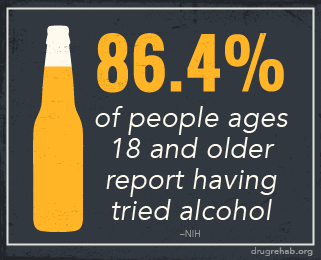
 Alcohol abuse
Alcohol abuse
 Alcohol withdrawals
Alcohol withdrawals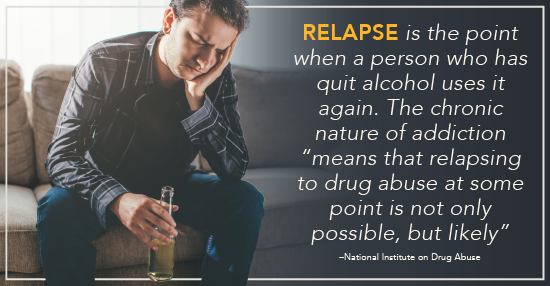
 In summary, alcohol withdrawal is not only a result of a physical demand of the chemical, but also the cognitive function in trying to maintain normal function.
In summary, alcohol withdrawal is not only a result of a physical demand of the chemical, but also the cognitive function in trying to maintain normal function.





 Temazepam is one of the many sedatives that can be used to help a person sleep, but in the illicit market, there’s a lot of room for diversion and abuse of it. Perhaps you’ve never heard of it, but temazepam a much bigger problem than most of us realize.
Temazepam is one of the many sedatives that can be used to help a person sleep, but in the illicit market, there’s a lot of room for diversion and abuse of it. Perhaps you’ve never heard of it, but temazepam a much bigger problem than most of us realize. Temazepam and other benzodiazepines are classified as schedule IV depressants by the
Temazepam and other benzodiazepines are classified as schedule IV depressants by the  During this time, you’ll gradually be taken off the benzodiazepine, and your withdrawal symptoms will be carefully monitored by professionals.
During this time, you’ll gradually be taken off the benzodiazepine, and your withdrawal symptoms will be carefully monitored by professionals.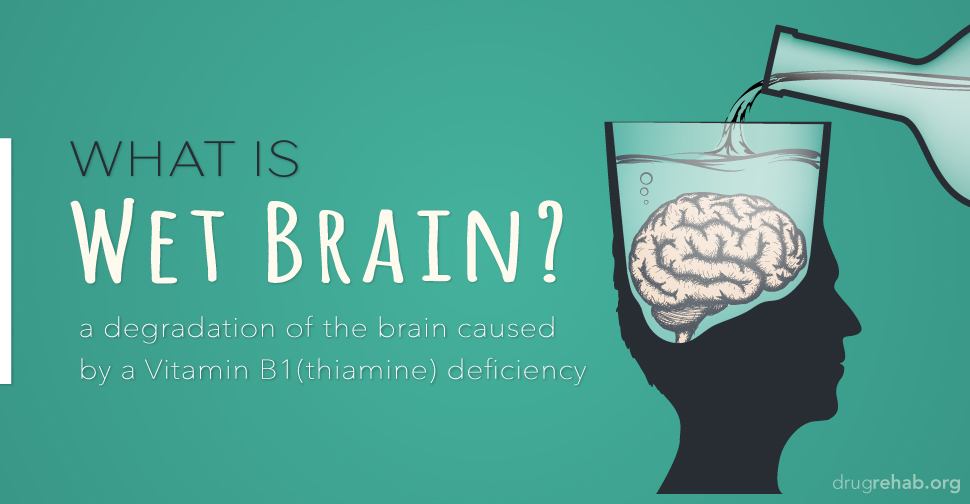


 The
The