When you suffer from post-traumatic stress disorder (PTSD), you experience a wide range of mental and physical health problems. Unfortunately, these problems often push a person to begin using drugs or alcohol in excessive amounts which can lead to an addiction. The common occurrence is a result of the complexity of the situation, as PTSD is a very individualized problem and one that affects people in different ways. Drug addiction is also complex, and when it’s paired with the negativity of PTSD, it creates a thick web that can be hard to escape. If you or someone you love suffers from dual diagnosis, you need to understand as much about it as possible in order to beat it.
In this in-depth look at dual diagnosis, PTSD, and substance abuse, we are going to delve deeply into the causes of these problems and how they interact with each other. We will take a look at research study data and teach you how to pin-point the moment when your PTSD started and how it led to addiction. When you finish reading, you will also understand how to best take care of your dual diagnosis and the effectiveness of its treatment methods.
What Is PTSD?
Before going deeper into this subject, let’s take a moment to fully understand PTSD. This is important because you may be uncertain if you have this problem or may be suffering from an undiagnosed case. While this information is not designed to be a medical diagnosis, it can help you get a better idea of whether you have it. Use this information with your personal doctor to come with a proper diagnosis.
The mental health advocacy group, Mental Health America, defined post-traumatic stress disorder in the following way: “Posttraumatic [sic] Stress Disorder (PTSD) is an anxiety disorder that can occur following the experience or witnessing of a traumatic event. A traumatic event is a life-threatening event such as military combat, natural disasters, terrorist incidents, serious accidents, or physical or sexual assault in adult or childhood.”
When a person experiences these situations, they develop symptoms that make their life more difficult, such as:
- Thinking constantly about the traumatic moment, including having nightmares about it
- Being on high alert or trying to feel overly protected from danger, even when it does not exist
- Being easily startled and often irritable about nothing in particular
- Staying away from friends, family members, or even locations related to the trauma
- Sudden increase in panic or anxiety, causing additional side effects like nausea, dizziness, and even blackouts
- Severe headaches, cramps, stomach pain, muscle cramps, and even lower back pains
- Difficulty trusting others and having personal and professional problems
- Suicidal thoughts that are fueled by the trauma and difficult to face
- Depression related to the trauma and an increased sense of hopelessness
- The development of other mental health disorders, such as bipolar disorder or schizophrenia
With this increased understanding of PTSD, you can better understand how it may be influencing your drug addiction.
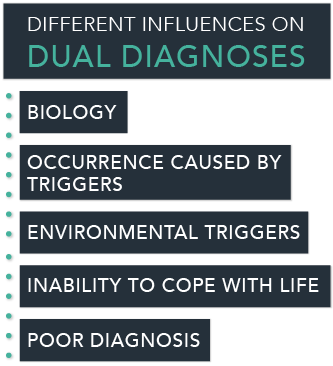
Where Dual Diagnoses Might Originate
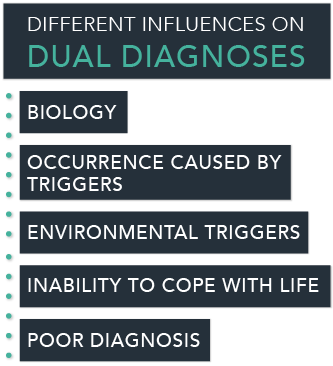
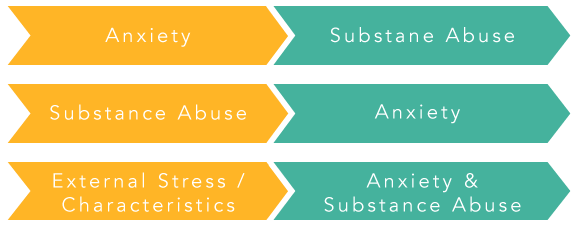
There are a variety of different influences on dual diagnosis and it is valuable to gain an understanding of how they may begin. A few of the most common are:
- Biology – People who suffer from mental health disorders are often genetically predisposed to these conditions. This may include “super sensitivity,” a problem that may lead to a higher occurrence of PTSD. It also includes increased sensitivity to dopamine and other chemicals.
- Occurrence caused by triggers – This is a situation caused by a substance triggering a latent disorder. For example, someone who has a predisposition towards bipolar disorder may trigger it by using substances. The same is true of disorders that may lead to PTSD.
- Inability to cope with life – Stress and anxiety often strip away a person’s patience and coping abilities. If they suffered from PTSD, coping abilities might be even more affected. In this situation, people often turn to substance abuse to alleviate their symptoms and feel more stable.
- Environmental triggers – Even a person with no mental health problems can develop one based on environment. This can result from a traumatic situation, such as losing both parents at a young age or perhaps losing a job and being threatened with bankruptcy.
- Poor diagnosis – Mental health disorders often have overlapping symptoms that can cause improper diagnosis. For this reason, a person who has a serious problem, like schizophrenia, may not get the medical attention that they need which may lead to self-medication with substance abuse.
As you can see, any of these situations might also be a contributor to PTSD. That problem occurs when a person experiences a traumatic situation that leaves them feeling drained, depressed, and defeated. Suddenly developing a mental health disorder could cause PTSD, especially if it shows itself in a dramatic manner. Struggling to cope with life and environmental triggers may also cause PTSD, creating an even higher chance of developing an addiction.
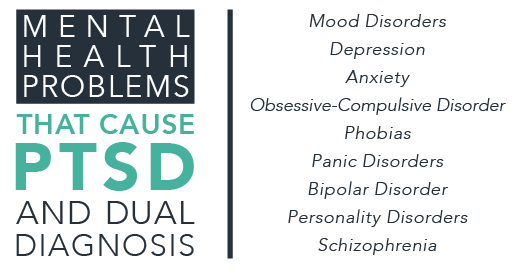
Mental Health Problems That Cause PTSD And Dual Diagnosis
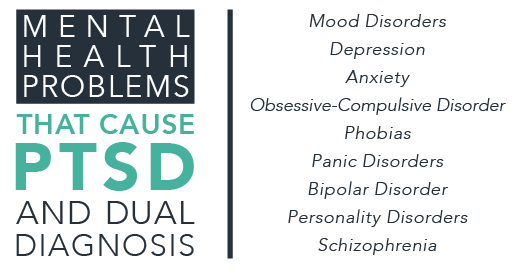
Mental health disorders come in a wide range and they each cause a great degree of personal struggle and difficulty. Many of these problems have the potential to cause PTSD and lead to dual diagnosis. While having one of the following mental health problems doesn’t necessarily mean someone will develop a dual diagnosis, it does increase the risk:
- Mood Disorders
- Depression
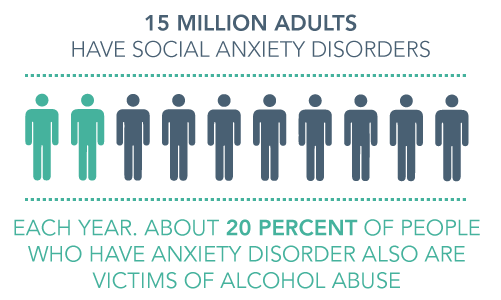
- Anxiety
- Obsessive-Compulsive Disorder
- Phobias
- Panic Disorders
- Bipolar Disorder
- Personality Disorders
- Schizophrenia
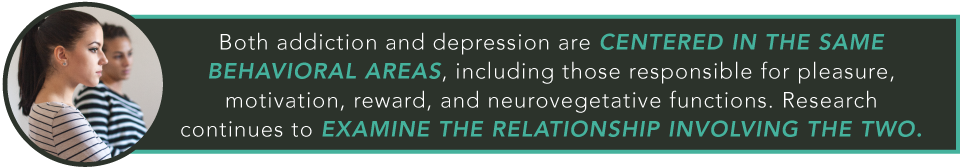
The increased risk of addiction that comes with each disorder varies. For example, people who suffer from antisocial personality disorder have a 15.5 percent increased risk of developing an addiction, those with mania have a 14.5 percent increase, and those with schizophrenia have a 10.1 percent increased risk. This elevated risk is caused by disease symptoms and their possibility of creating PTSD.
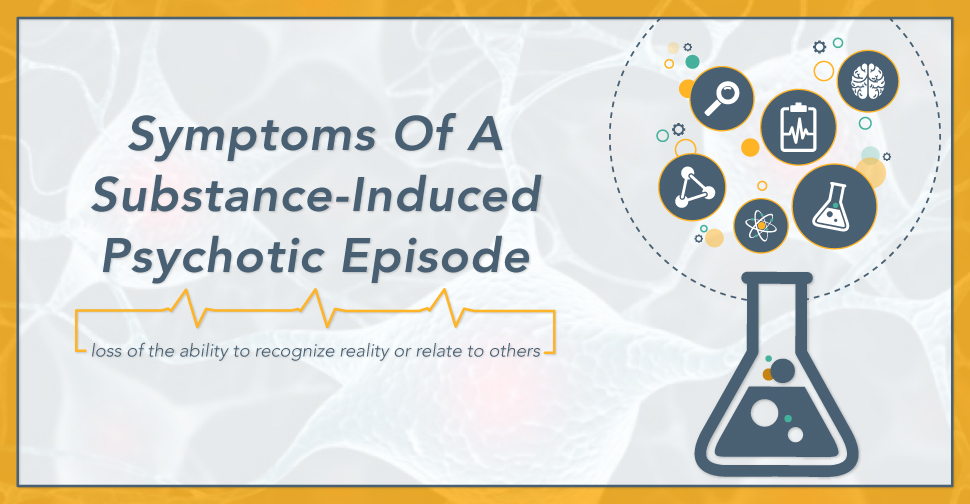
For example, a person with schizophrenia may develop their symptoms suddenly and experience a traumatic break from reality. This can cause PTSD symptoms to occur alongside their schizophrenia, further increasing the risk of addiction. However, PTSD and depression are heavily linked, just like depression is with many other disorders, and understanding where depression begins and how it influences PTSD is crucial to further assessing your dual diagnosis situation.
Breakdown Of The Various Theories Of Depression
Depression, like PTSD and other mental health disorders, develops in a variety of ways. Fully grasping these points of development can be important in treating your dual diagnosis and eliminating the negative influence of PTSD and addiction from your life. One of the most common causes of depression is chemical, a problem that Richard H. Hall of Missouri S&T University delves into in his short paper “Theories of Depression.”
Hall states that people with chemical depression often have an underactive production of monoamines, which are chemicals that help promote happiness and stability. He found that people who had low levels of this chemical suffered from severe depression.
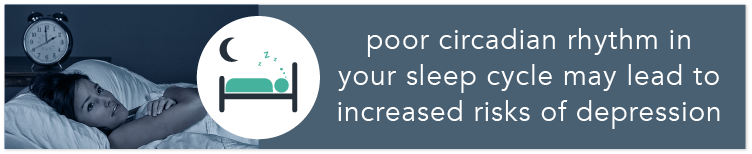
Another theory he posits includes the effect of poor circadian rhythm in your sleep cycle. The idea is that an unhealthy sleep cycle may lead to increased risks of depression. This is particularly true of people who suffer from low instances of REM or dream-state sleep. His studies found that those who were sleep deprived in a laboratory setting often developed depression symptoms which were not there before.
Beyond these concepts is the behaviorist theory which is the idea that our environment and its influence on us is what leads to depression. Depression is, in this belief, nothing but the result of negative behavior patterns that resulted from learned behaviors in specific situations. For example, if a person who is overweight was teased for it as a young child, they may associate being heavy with negativity. This may cause them to fall into depression if they struggle with their weight.
This theory is also related to the idea of “learned helplessness” or the idea that people with depression learn how to be “helpless” and depressed at a young age. This might have occurred when a child learned to cry to get what they wanted or to claim an inability to perform a simple act, such as tying their shoes. Later in life, they may struggle to break this helplessness and feel that escaping from negative situations on their own is beyond them, further fueling their depression.
What is interesting about the latter idea is how it relates to PTSD. People who suffer from PTSD may experience a state of helplessness in the moment of their traumatic experience. As a result, they may fall into a state of learned helplessness which is new to them and which is hard for them to manage.
The Connections Between PTSD, Depression, And Co-Occurring Disorders
The connections that link these disorders are very complex, but not impossible to understand. As mentioned before, PTSD is heavily linked to depression and other mental health disorders. People who suffer from these problems may not even realize they are and may try to continue going on with their life as normal. This might include drinking alcohol or occasionally engaging in drug use.
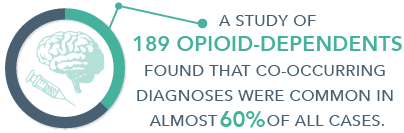
Unfortunately for the nearly eight million Americans who have PTSD, this may lead to an increased risk of turning to drugs as a way of self-medicating the negative effects of depression, PTSD, and other mental health disorders. As PTSD often exacerbates these mental health disorders, it can create an even tighter and more difficult to escape dual diagnosis. This idea was tested in a study entitled “Cognitive Distortions In The Dual Diagnosis Of PTSD And Substance Use Disorder,” particularly the way that cognitive ideas caused by PTSD led to dual diagnosis.
The study sampled 102 women with PTSD and a substance use disorder and 27 women who just had PTSD. They found that PTSD led to an increased risk of depression, anxiety, and drug addiction. Thankfully, they also found that many of the treatment methods applicable for both cases were effective in eliminating many of the problems associated with the dual diagnosis of PTSD and addiction.
Why do PTSD and substance use disorders mesh together so well in such a negative way? There are a variety of influences. For example, a person with PTSD may have troubles sleeping and may turn to alcohol or other calming drugs to fall asleep. Or they may have the opposite problem and feel numb and without energy. Stimulants, such as cocaine or meth, may give them the energy they need to face the concerns of day-to-day life.
Even worse is the way that PTSD can fuel thoughts of depression and avoidance. Drinking alcohol and taking drugs may distract the mind from its depression and further fuel the avoidance of the negative memories associated with trauma. Sadly, these effects won’t last for long, which will cause a person to turn to increasing doses of substances in order to stay stable, happy, and comfortable.
The Connection Has Been Studied
The study of the influence of these two disorders was focused on in “Posttraumatic (sic) Stress Disorder And Co-Occurring Substance Use Disorders: Advances In Assessment And Treatment,” a paper published by the National Center For Biotechnology Information. In it, the researchers came to a sad, but important to understand conclusion:
 “The comorbid presentation of PTSD and SUDs is remarkably common, and in comparison to patients presenting with either PTSD or SUD alone, PTSD/SUD patients often report greater functional impairment and experience poorer treatment outcomes –including treatment failure and dropout. Several mechanisms have been posited to explain the co-occurrence of PTSD and SUDs, including the self-medication hypothesis, the high-risk hypothesis, the susceptibility hypothesis. The majority of research to date supports the self-medication hypothesis.”
“The comorbid presentation of PTSD and SUDs is remarkably common, and in comparison to patients presenting with either PTSD or SUD alone, PTSD/SUD patients often report greater functional impairment and experience poorer treatment outcomes –including treatment failure and dropout. Several mechanisms have been posited to explain the co-occurrence of PTSD and SUDs, including the self-medication hypothesis, the high-risk hypothesis, the susceptibility hypothesis. The majority of research to date supports the self-medication hypothesis.”
What this indicates is clear: people with PTSD most often use substances to self-medicate the negative influence of their disorder. This causes an increase in usage and even addiction, which is only fueled by the continued occurrence of these disorders. That’s why it’s so important to understand how to treat them, as this can help you break a negative feedback cycle and learn how to live a healthy life.
Eliminating PTSD
PTSD has become such a major problem that a variety of treatment methods have been created to help treat its negative symptoms. The most common of these are various methods of psychotherapy, including talk therapy, individual assessment, group therapy, and family counseling. Often people who suffer from PTSD interact well with others who have experienced a similar trauma, as they can relate and better understand each other.
Psychotherapy can also include methods such as cognitive behavioral therapy, which helps you identify the negative thought and behavior patterns in your life. By identifying these negative patterns with a skilled therapist you can replace them with positive ones. For example, if your PTSD has you on edge and nervous about another occurrence of trauma, cognitive behavioral therapy can help you learn to substitute those reactions with positive and relaxing ones.
Exposure therapy is also often used to treat PTSD and it is exactly what it sounds like: you are exposed to the situation which caused your trauma. Obviously this is done in a safe environment and it is designed to help you face your fear and beat it. New virtual reality treatments are often available for this therapy, completely eliminating any danger from the real situation.
Another interesting treatment is eye movement desensitization. This method works with exposure therapy to track your eye movements in order to understand how you are processing your traumatic memories. By teaching you new guided eye movements, you will learn how to better handle your traumatic memories and avoid letting them pull you back into addiction.
Beyond these psychotherapy methods are a variety of medications that treat the depression and anxiety symptoms that come with PTSD. These include antidepressants, anti-anxiety medications, prazosin (a drug that helps suppress nightmares associated with PTSD), and more. The idea here is to carefully guide you through these negative emotions, balance your emotional health, and give you the strength you need to fight the negative influences of PTSD.
Why Treating Both At The Same Time Is Most Effective
While it is possible to treat PTSD separately from your addiction, it’s fair to say that it’s best to treat both at the same time. Why? The two are so intricately mixed that it can be hard to treat them individually. For example, if you just try to treat addiction without handling PTSD, the anxiety and depression caused by the latter problem may influence a relapse. Conversely, trying to beat PTSD while still nursing an addiction will only fuel the intensity of the problems it causes.
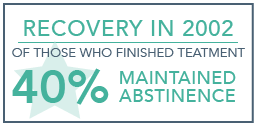
We come to this conclusion after understanding multiple studies that tested dual diagnosis or co-occurring disorder therapies and which concluded that treating both simultaneously was the best option. For example, a study entitled “Treatments For Patients With Dual Diagnosis: A Review” concluded that “… existing efficacious treatments for reducing psychiatric symptoms also tend to work in dual-diagnosis patients (and) existing efficacious treatments for reducing substance use also decrease substance use in dually diagnosed patients…”
Essentially, this means that treatments for addiction also work well for people who have mental health problems. This indicates that treating both is not only possible, but preferable, as it is possible to eliminate both problems by utilizing the same treatment methods. Perhaps that’s why BMC Psychiatry, in a study on dual diagnosis client treatment satisfaction, found that “… integrated DD treatment yielded greater client satisfaction than standard treatment without explicit DD focus. In standard treatment without DD focus, DD clients tended to be less satisfied than single diagnosis clients.”
While these studies weren’t necessarily examining PTSD as a dual diagnosis specifically, the promising results they suggested show that dual diagnosis treatments for both mental health disorders and addiction can serve as an appropriate and effective way to eliminate both problems. So please consider making the investment, both in time and money, and helping yourself beat addiction for good.
Finding Appropriate Treatment For Your Needs
If you suffer from PTSD and a drug addiction, there is good news, as multiple drug rehab centers across the nation now focus heavily on dual diagnosis treatment. The rigors and difficulties of modern life have made trauma more of a problem than ever, and rising addiction rates may reflect this reality. It doesn’t matter where your addiction or your PTSD originated: dual diagnosis treatments can help you.
But how do you find a center near you that is willing to help? You could search online and read through a variety of addiction center listings. This may be effective if you are looking to get into a rehab center quickly, but you might be leaving out a drug center in another state that might be more appropriate for your needs. For example, if you are a mother suffering from PTSD caused by childbirth, there may be a center thousands of miles away that focuses on this specific concern.
That’s why reaching out to us at DrugRehab.org can help you begin your journey. Our addiction therapy specialists know all too well how addiction and  PTSD can impact your life. They understand the myriad of influences PTSD and depression has on your life and will work hard to find you a center that works specifically for you. Please don’t hesitate to reach out to us today to experience the healing power of recovery. Contact us today, we are here to help!
PTSD can impact your life. They understand the myriad of influences PTSD and depression has on your life and will work hard to find you a center that works specifically for you. Please don’t hesitate to reach out to us today to experience the healing power of recovery. Contact us today, we are here to help!
Sources
University Of Utah – Mental Illness: The Challenge Of Dual Diagnosis
Mental Health America – Post-Traumatic Stress Disorder
NHS Choices – Dual Diagnosis
Missouri S&T University – Theories Of Depression
Simply Psychology – Psychological Theories Of Depression
Anxiety And Depression Association Of America – Post-Traumatic Stress Disorder
Springer Link – Cognitive Distortions In The Dual Diagnosis Of PTSD And Substance Use Disorder
National Institute On Drug Abuse – Comorbidity: Addiction And Other Mental Illnesses
U.S. Department Of Veterans Affairs – PTSD And Substance Abuse In Veterans
Mayo Clinic – Post-Traumatic Stress Disorder: Treatments And Drugs
National Institute On Drug Abuse – Treatments For Patients With Dual Diagnosis: A Review
BMC Psychiatry – Dual Diagnosis Clients’ Treatment Satisfaction – A Systematic Review




 Fighting cancer can be a pretty scary business, and the pain it causes can be unbearable; someone who is suffering a terminal illness like cancer is likely to be in unimaginable pain. Pain is actually reported to be the biggest fear of someone suffering from cancer; not death, and not the loss of their life, but pain. For a person suffering with an often incurable condition, sometimes the only thing medical professionals can do is give them painkillers and anxiety medication to help them feel comfortable.
Fighting cancer can be a pretty scary business, and the pain it causes can be unbearable; someone who is suffering a terminal illness like cancer is likely to be in unimaginable pain. Pain is actually reported to be the biggest fear of someone suffering from cancer; not death, and not the loss of their life, but pain. For a person suffering with an often incurable condition, sometimes the only thing medical professionals can do is give them painkillers and anxiety medication to help them feel comfortable.
 The medical fraternity has come a long way in treating an addiction. Sometimes
The medical fraternity has come a long way in treating an addiction. Sometimes 
 Narcissism is rarely a desired attribute, though it is often directly related to a personality disorder. Personality disorders fall into the
Narcissism is rarely a desired attribute, though it is often directly related to a personality disorder. Personality disorders fall into the 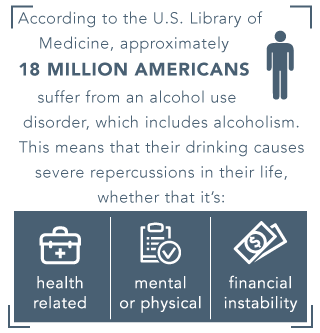 According to the
According to the  A person who is suffering from alcoholism and narcissistic personality disorder, might answer the question (How the heck aren’t you drunk yet?), with a false sense of pride or by stating anything other than “because I can’t stop drinking”, or by stating, “I have built up a tolerance.” There are many accomplishments that deserve a person the right to be proud of themselves, but unfortunately, alcoholism is not one of them, and it’s dangerous to believe that it is. Intervention and treatment are very likely the only way to get a person on the right track towards recovery. Try to remember that Alcoholism is a disease and the person with it is very sick.
A person who is suffering from alcoholism and narcissistic personality disorder, might answer the question (How the heck aren’t you drunk yet?), with a false sense of pride or by stating anything other than “because I can’t stop drinking”, or by stating, “I have built up a tolerance.” There are many accomplishments that deserve a person the right to be proud of themselves, but unfortunately, alcoholism is not one of them, and it’s dangerous to believe that it is. Intervention and treatment are very likely the only way to get a person on the right track towards recovery. Try to remember that Alcoholism is a disease and the person with it is very sick.
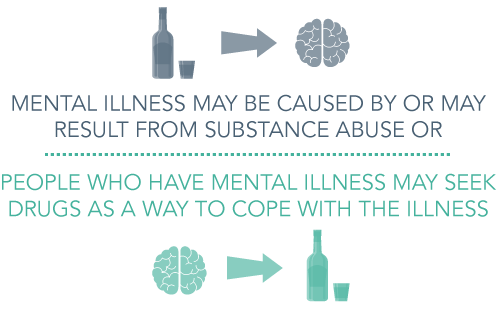
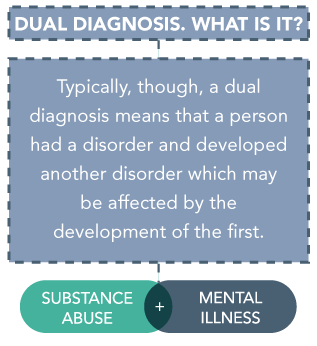 People affected by dual diagnosis may experience dire effects to their health; each disease can greatly influence the other, and either disease can occur first. Further, the problem of dual diagnosis is vast. As NAMI reports, “about a third of all people experiencing mental illnesses and about half of people living with severe mental illnesses also experience substance abuse.” The reverse is also true, as nearly the same amount of people affected by substance abuse are suffering from mental illness as well.
People affected by dual diagnosis may experience dire effects to their health; each disease can greatly influence the other, and either disease can occur first. Further, the problem of dual diagnosis is vast. As NAMI reports, “about a third of all people experiencing mental illnesses and about half of people living with severe mental illnesses also experience substance abuse.” The reverse is also true, as nearly the same amount of people affected by substance abuse are suffering from mental illness as well.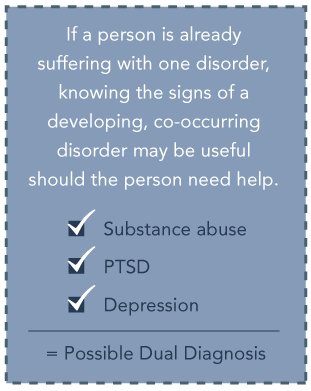 Symptoms of mental illness are great in number, but some may signal the development of a disorder. A person with a developing mental illness may have problems concentrating at school or work, undergo severe mood changes, withdraw from family or friends, or have
Symptoms of mental illness are great in number, but some may signal the development of a disorder. A person with a developing mental illness may have problems concentrating at school or work, undergo severe mood changes, withdraw from family or friends, or have 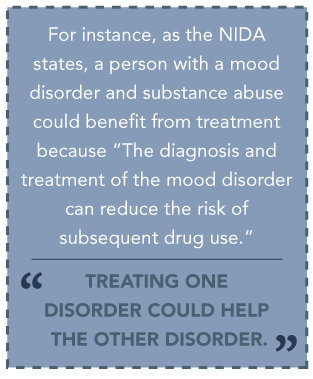 Some of the best treatments can occur in an
Some of the best treatments can occur in an 


 One of the most important things to remember about
One of the most important things to remember about 



 “The comorbid presentation of PTSD and SUDs is remarkably common, and in comparison to patients presenting with either PTSD or SUD alone, PTSD/SUD patients often report greater functional impairment and experience poorer treatment outcomes –including treatment failure and dropout. Several mechanisms have been posited to explain the co-occurrence of PTSD and SUDs, including the self-medication hypothesis, the high-risk hypothesis, the susceptibility hypothesis. The majority of research to date supports the self-medication hypothesis.”
“The comorbid presentation of PTSD and SUDs is remarkably common, and in comparison to patients presenting with either PTSD or SUD alone, PTSD/SUD patients often report greater functional impairment and experience poorer treatment outcomes –including treatment failure and dropout. Several mechanisms have been posited to explain the co-occurrence of PTSD and SUDs, including the self-medication hypothesis, the high-risk hypothesis, the susceptibility hypothesis. The majority of research to date supports the self-medication hypothesis.”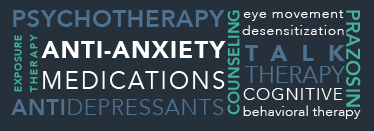




 A typical codependent relationship consists of one person who uses the other to achieve their own personal needs. For example, in a relationship with drug addiction, the person addicted might manipulate their partner to get drugs or provide a place in which to live. It goes beyond merely getting help, though, and becomes a way to justify and enable negative behaviors, such as continued drug use.
A typical codependent relationship consists of one person who uses the other to achieve their own personal needs. For example, in a relationship with drug addiction, the person addicted might manipulate their partner to get drugs or provide a place in which to live. It goes beyond merely getting help, though, and becomes a way to justify and enable negative behaviors, such as continued drug use. Basically, drug use forces your loved one to become reliant on you in an almost child-like way. You need to buy them food (and drugs), give them a place to live, drive them where they need to go, and provide constant companionship. They will want to know where you’re at at all times and are likely to demand difficult things from you in order to make you “prove your love.”
Basically, drug use forces your loved one to become reliant on you in an almost child-like way. You need to buy them food (and drugs), give them a place to live, drive them where they need to go, and provide constant companionship. They will want to know where you’re at at all times and are likely to demand difficult things from you in order to make you “prove your love.” Codependency is a bad cycle that can seem impossible to break. If you’re in a codependent relationship, you know the kind of emotional and even physical bonds they impose. Breaking through a codependent cycle is the first step in getting your loved one help and the initial phase in that process is identifying the causes of codependency. Codependency has a wide variety of causes, including:
Codependency is a bad cycle that can seem impossible to break. If you’re in a codependent relationship, you know the kind of emotional and even physical bonds they impose. Breaking through a codependent cycle is the first step in getting your loved one help and the initial phase in that process is identifying the causes of codependency. Codependency has a wide variety of causes, including: Once you’ve got your loved one ready to accept help for their addiction, you need to do what you can to help keep them out of the rut of addiction. This is also crucial for your personal needs as you have to identify the traits that allowed you to fall into this type of relationship and how you can avoid it in the future.
Once you’ve got your loved one ready to accept help for their addiction, you need to do what you can to help keep them out of the rut of addiction. This is also crucial for your personal needs as you have to identify the traits that allowed you to fall into this type of relationship and how you can avoid it in the future.

 Szalavitz suggests that defining
Szalavitz suggests that defining