While drug abuse of any kind can be dangerous, certain routes of administration can cause greater damage than others. Intravenous drug use, the act of injecting a water-soluble drug into one’s body, is one of the most invasive and dangerous ways an individual can administer a drug. Through continued use and repeated trauma to the injection site, IV drug abuse leads to many hazardous health effects, including sepsis.
What Is Sepsis?
While many people think sepsis is an infection itself, it’s actually a complication caused by an infection. As explained by Mayo Clinic, “sepsis occurs when chemicals are released into the bloodstream to fight the infection trigger inflammatory responses throughout the body.”
The type of infection which can cause sepsis varies. Sepsis is most heavily linked to bacteria, though certain forms of fungus or viruses may also cause it. Sepsis is commonly referred to as “blood poisoning,” as the bacteria or toxins produced by them overtake the bloodstream.
What Are The Stages Of Sepsis?
Mayo Clinic explains that sepsis is typically broken down into three stages:
Sepsis
Sepsis is diagnosed only when there is reasonable suspicion or verification of an infection, in addition to two of the following symptoms:
- Body temperature above 101 F (38.3 C) or below 96.8 F (36 C)
- Heart rate higher than 90 beats a minute
- Respiratory rate higher than 20 breaths a minute
Severe Sepsis
Within this state, a person must have one or more of the following symptoms:
- Improperly working heart
- Respiratory (breathing) struggles
- Pain in the abdomen
- Platelet count begins falling
- Rapidly altered mental states
- Urine production drastically drops
Any of these symptoms indicate potential organ failure.
Septic Shock
As a person’s condition advances to this state, they will display the above signs and symptoms. But, in order to qualify as septic shock, a person’s blood pressure must remain low despite attempts to increase it with fluid replacement.
Sepsis becomes more dangerous as it progresses through these stages. To avoid the greatest danger, treatment should begin as early as possible.
How Does IV Drug Use Cause Sepsis?
Intravenous drug use can introduce numerous toxins and pathogens into a person’s veins and body at large, which pave the way for infection. Pathogens include bacteria, fungi, and viruses. Staphyloccus aureus, or MRSA as it’s better known to most of us, is the bacteria most frequently responsible for IV drug infections.
Transmission of these pathogens often occurs due to improper and unhygienic handling of needles. As a person becomes addicted, the need to use becomes so intense that they disregard their health. Because of this, some users share needles. This behavior increases the risk that a pathogen will be transmitted by blood-to-blood contact.

Even if you never share needles, you could still be at risk. Far too many drug abusers repeatedly use the same syringe. Doing so allows bacteria to grow on the needle, which could then be transmitted into your tissue and blood. Even with new needles, a person can still get an infection if they don’t properly clean the injection site. Research has found that bacteria from a person’s skin presents a greater risk than that which is present on shared needles.
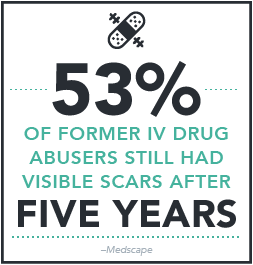
Intravenous injection requires a vein, which leaves drug abusers with only so many options. Because of this, many users will repeatedly inject at the same site. This can create abscesses, track marks, or ulcers, all of which can lead to serious infection. Sometimes, a user will actually miss the vein and inject the drug into their muscle or right under the skin, raising the risk of infection in these regions. Lastly, it’s suspected that using black tar heroin increases a user’s risk of infection.
What Types Of IV Drug-Related Illness Or Disease Cause Sepsis?
Intravenous drug abuse causes a range of infections, many of which can become deadly. One of the biggest reasons why these infections endanger a person’s life is because they cause sepsis.
The following infections can lead to sepsis:
Cellulitis: This infection affects both the skin and underlying tissue, and can spread outwards across the limb.
Endocarditis: This occurs when bacteria, fungus, or viruses cause an infection within your heart’s inner lining and valves.
Necrotizing fasciitis: Often referred to as the “flesh-eating disease,” this rare but serious infection is extremely aggressive and causes your body’s soft tissues to die.
Whether you inject sporadically or chronically, you’re exposing yourself to danger. While it’s true that prolonged and chronic use increases your risk over time, it is possible to contract an infection from even one use.
What Are The Complications And Dangers Of Sepsis?
Sepsis poisons your blood and body. The more time that passes without treatment, the greater the risk of complications and fatality. Sepsis can become so severe that your organs struggle to function properly. This can lead to organ damage and/or failure. Combined with the dangers of the infections themselves, these effects even further increase the risk of death.
A person’s veins can become septic and develop blood clots, inflammation, and bacteria throughout. Injecting into the jugular or other central veins increases this risk. These states could develop into sepsis and septic emboli (bacteria and pus-filled embolisms), both of which can be life-threatening conditions.
As outlined by the Sepsis Alliance, individuals who recover from sepsis often face serious long-term effects, such as:
- Amputated limbs
- Chronic pain
- Chronic fatigue
- Post-traumatic stress disorder (PTSD)
- Organ dysfunction
How Is Sepsis Treated?
If you suspect you have or are developing sepsis, seek medical help immediately. Left untreated, sepsis can progress rapidly to the point of threatening your life. As soon as you seek treatment, medical staff will likely administer a broad-spectrum antibiotic. This medication can address various types of infection and the bacteria which cause them. Once tests determine the specific bacteria, a more focused antibiotic may be used.
Through these stages, Mayo writes that other treatments may be initiated, such as:
- Corticosteroids
- Drugs to stabilize the immune system
- Insulin (to stabilize blood sugar)
- IV fluids
- Oxygen
- Painkillers (staff should proceed accordingly with opioid-addicted individuals)
- Sedatives
- Vasopressor medication to raise blood pressure
Advanced stages of sepsis may require:
- Breathing support
- Kidney dialysis
- Surgery
Mayo Clinic cautions that “people with severe sepsis require close monitoring and treatment in a hospital intensive care unit. If you have severe sepsis or septic shock, lifesaving measures may be needed to stabilize breathing and heart function.”
While sepsis can be treated, we urge you to consider preventative measures to avoid this risk. Effective drug rehab can help you to overcome your IV drug addiction. Here you’ll encounter counseling, behavioral therapies, and if needed, medication-assisted treatment. Along with other dynamic modalities, these things can help you overcome your addiction.
Don’t Let IV Drug Abuse Destroy Your Health Or Claim Your Life
Contact Drugrehab.org today if your or a loved one is struggling with an addiction to drugs or alcohol. Our treatment specialists can help find a program that is tailored to your needs. If you suspect that yourself or a loved one may have sepsis or another serious infection as a result of intravenous drug use contact your doctor or go to a hospital immediately.



 Again, cotton balls are commonly used for this purpose since they are so cheap and readily available. Once a drug is in liquid form, a person draws the substance through the filter and into the syringe. The forearm is a
Again, cotton balls are commonly used for this purpose since they are so cheap and readily available. Once a drug is in liquid form, a person draws the substance through the filter and into the syringe. The forearm is a 
 Immunologic theory: Users have antibodies for the cotton which cause a reaction after injection
Immunologic theory: Users have antibodies for the cotton which cause a reaction after injection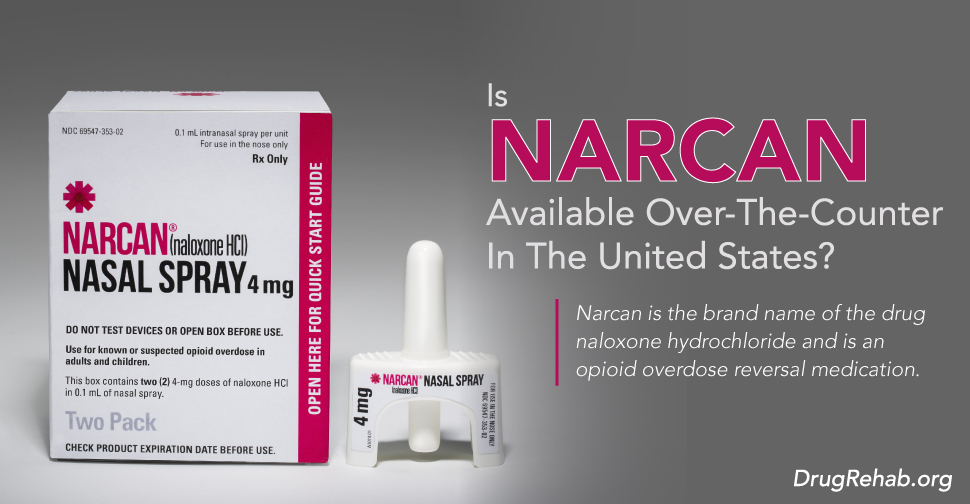
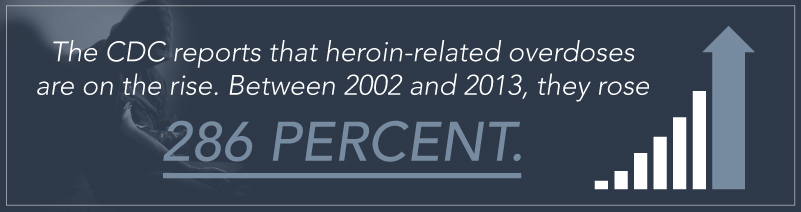
 Additionally, a person who is experiencing overdose themselves may not be able to administer the Narcan. Even then, chronic opioid abusers should keep Narcan on or near them. It’s important the user notifies those close to them of the location of this drug, so that these individuals have access to it fast. The prescribing doctor or pharmacist (if purchased over-the-counter) can walk you through using Narcan.
Additionally, a person who is experiencing overdose themselves may not be able to administer the Narcan. Even then, chronic opioid abusers should keep Narcan on or near them. It’s important the user notifies those close to them of the location of this drug, so that these individuals have access to it fast. The prescribing doctor or pharmacist (if purchased over-the-counter) can walk you through using Narcan.
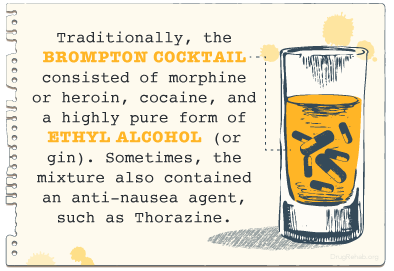 As previously mentioned, the Brompton Cocktail consists of a few different substances, meant to give ultimate relief from pain. Traditionally, the Brompton Cocktail consisted of morphine or
As previously mentioned, the Brompton Cocktail consists of a few different substances, meant to give ultimate relief from pain. Traditionally, the Brompton Cocktail consisted of morphine or 
 Treatment for any type of addiction has to be comprehensive. Addiction doesn’t just affect your physical health, but actually changes the way you think and behave, so treatment for it must address these changes and work to better them. This is especially true when dealing with addiction to more than one substance.
Treatment for any type of addiction has to be comprehensive. Addiction doesn’t just affect your physical health, but actually changes the way you think and behave, so treatment for it must address these changes and work to better them. This is especially true when dealing with addiction to more than one substance.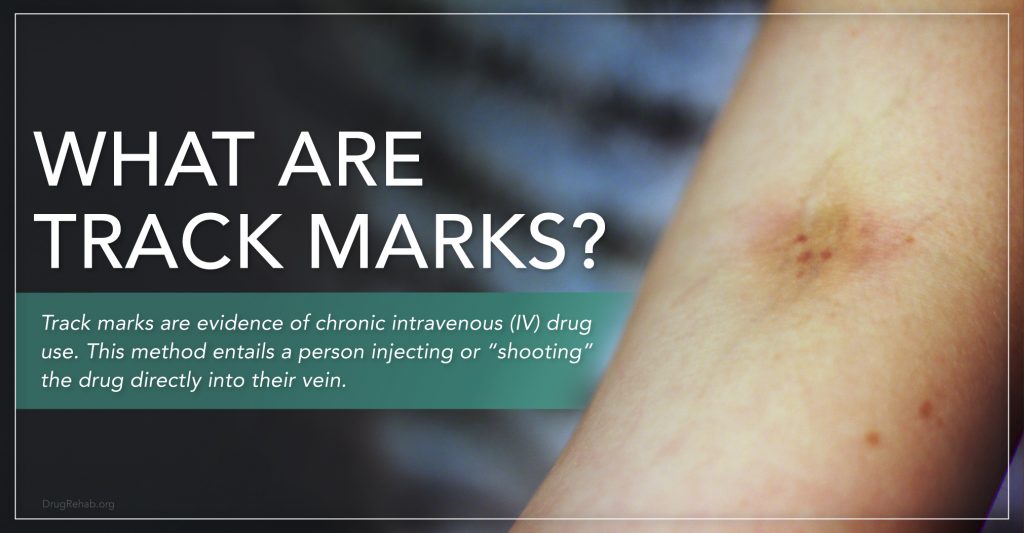
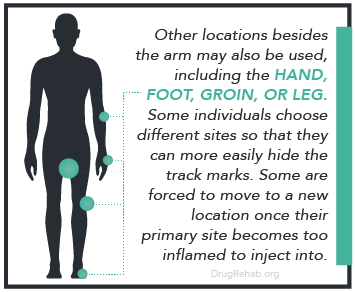 The most frequently used veins are those in the crook of the forearm, though other locations may be used. If a person injects into their arm, it’s typically the one opposite from the hand they write with. This makes it easier for them to inject the drug themselves. To work around this, some people may have a fellow drug abuser inject the substance for them into their dominant arm.
The most frequently used veins are those in the crook of the forearm, though other locations may be used. If a person injects into their arm, it’s typically the one opposite from the hand they write with. This makes it easier for them to inject the drug themselves. To work around this, some people may have a fellow drug abuser inject the substance for them into their dominant arm.
 Injection drug users face increased risk of blood-borne infectious diseases, such as HIV/AIDS and Hepatitis B and C.
Injection drug users face increased risk of blood-borne infectious diseases, such as HIV/AIDS and Hepatitis B and C.
 Since then the coca plant has grown in popularity among the rest of the world, especially since
Since then the coca plant has grown in popularity among the rest of the world, especially since 

 When a drug abuser injects a drug, they need certain equipment. These items are collectively termed paraphernalia. Finding these objects can be a telltale sign that a person is engaging in IV drug use. The most obvious one would be a syringe (insulin syringes are frequently used). You might also find pill bottles, baggies, or balloons which contained the drugs.
When a drug abuser injects a drug, they need certain equipment. These items are collectively termed paraphernalia. Finding these objects can be a telltale sign that a person is engaging in IV drug use. The most obvious one would be a syringe (insulin syringes are frequently used). You might also find pill bottles, baggies, or balloons which contained the drugs.




 The FDA sums it up perfectly, “abuse is characterized by misuse of the drug for nonmedical purposes, often in combination with other psychoactive substances. Physical dependence is a state of adaptation that is manifested by a specific withdrawal syndrome that can be produced by abrupt cessation, rapid dose reduction, decreasing blood level of the drug and/or administration of an antagonist…Tolerance is a state of adaptation in which exposure to a drug induces changes that result in a diminution of one or more of the drug’s effects over time.”
The FDA sums it up perfectly, “abuse is characterized by misuse of the drug for nonmedical purposes, often in combination with other psychoactive substances. Physical dependence is a state of adaptation that is manifested by a specific withdrawal syndrome that can be produced by abrupt cessation, rapid dose reduction, decreasing blood level of the drug and/or administration of an antagonist…Tolerance is a state of adaptation in which exposure to a drug induces changes that result in a diminution of one or more of the drug’s effects over time.”
 As the
As the 






 As young children, we look up to our parents, older peers, and other adults. While social learning is a primary concern with children, it doesn’t stop when we grow up. As we get older, our social influences include other family members, friends, and coworkers.
As young children, we look up to our parents, older peers, and other adults. While social learning is a primary concern with children, it doesn’t stop when we grow up. As we get older, our social influences include other family members, friends, and coworkers.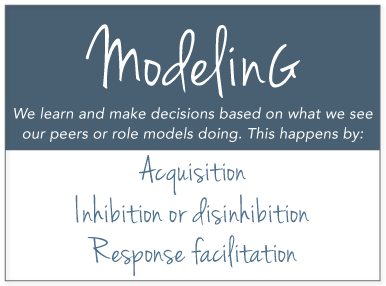 Self-Regulation: Our attitudes, beliefs, expectations, and perceptions of these circumstances shape how we relate our environment to our behaviors. Our understanding of this relationship alters how we self-regulate our future behaviors.
Self-Regulation: Our attitudes, beliefs, expectations, and perceptions of these circumstances shape how we relate our environment to our behaviors. Our understanding of this relationship alters how we self-regulate our future behaviors.